Atrial Septal Defects: Matthew’s Story
Atrial Septal Defects: Matthew’s Story
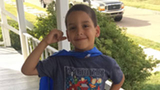
When 7-year-old Matthew sees his CHOP cardiologist for checkups, he swoops into the exam room like a superhero, his blue “heart hero” cape draped over his shoulders.
The cape isn’t just a costume — it’s a breakthrough.
Just a few years ago, Matthew, who had open heart surgery at age 3, felt embarrassed about the scar on his chest. But today, says his mother, Maria, “He shows off his scar every chance he gets. He knows what he went through was something major, and he’s very proud of it.”
Diagnosis: atrial septal defects
Matthew’s heart story began when he was just a week old. During a routine checkup at CHOP Primary Care in Kennett Square, PA, his pediatrician, Henry Karsch, DO, found that Matthew had a heart murmur. Dr. Karsch referred Matthew to pediatric cardiologist Richard Donner, MD, at the CHOP Specialty Care and Surgery Center in Exton.
At first, Maria wasn’t too worried. “I didn’t think it was a big deal,” she says. “I thought it was going to be something they would just monitor every now and then.”
But when an echocardiogram revealed that Matthew had several atrial septal defects (ASDs), everything changed.
“There was not a day that I didn’t think about it,” says Maria. “I wanted to put him in bubble wrap, but Dr. Donner told me he would be OK and to treat him like a normal kid.”
Follow-up care and additional testing
Because some atrial septal defects — also known as “holes in the heart” in the wall between the upper two chambers — close on their own, Dr. Donner recommended that Matthew be monitored closely.
During a follow-up visit a year later, though, tests revealed that the holes had gotten bigger. After further monitoring, Dr. Donner told Maria that Matthew would need a cardiac catheterization or open heart surgery to repair the holes.
Matthew’s medical team, including interventional cardiologist Yoav Dori, MD, initially believed that cardiac catheterization would be the best choice for Matthew.
The plan was to use a catheter (a long, thin tube that is threaded through a vein and into the heart) to place tiny closure devices in Matthew’s ASDs. But based on the results of a special imaging test performed in the catheterization lab, the team determined that Matthew’s best option was, in fact, open heart surgery.
Open heart surgery
In late April 2013, Matthew had open heart surgery to close his ASDs. His surgeon, Stephanie Fuller, MD, is one of four cardiothoracic surgeons at the Cardiac Center, which also has one of the nation’s only anesthesia teams focused specifically on pediatric cardiac patients. The surgical team performs more than 850 cardiothoracic surgeries a year, with outcomes among the best in the nation.
“The doctors were so reassuring,” says Maria. “Dr. Fuller is amazing. She is a great person and a great surgeon. I couldn’t have asked for anything better.”
Matthew spent a week at CHOP recovering from his surgery. During his stay, he received frequent visits from the Cardiac Center’s Child Life, Education and Creative Arts Therapy staff, who specialize in helping children cope with the hospital experience.
“They made sure he had toys and Play-Doh when he was ready to play,” says Maria. “And before he fell asleep, they made sure he had a DVD to watch.”
Maria was also impressed with the nurses who cared for Matthew: “They were just so nice to him. They did anything they could to make him happy and comfortable.”
Ongoing care
Matthew continues to come to CHOP for follow-ups, and when he gets older, he’ll be able to transition his care to the Philadelphia Adult Congenital Heart Center, a joint program of CHOP and Penn Medicine that provides care for adults with congenital heart disease.
Like most children who have had an ASD repaired, Matthew is leading a full and healthy life. He enjoys playing baseball and riding his miniature go-kart, and loves tractors and cars.
“He’s realizing what a strong kid he is,” says Maria. “He has an ‘I can do this’ attitude because he went through such an extreme surgery. He’s a brave kid who wants to do everything.”
Updated October 2016
Support Our Next Breakthrough
Philanthropic gifts to the Cardiac Center are vital to making breakthrough stories like Matthew's a reality. With your support, we can provide innovative care, pioneering treatments and lifesaving cures to more children — today, tomorrow and for years to come.