
Heart transplant policies underwent significant changes in 2016 and 2018, altering how hearts are allocated to patients waiting for a transplant. These changes aimed to improve survival rates and outcomes for patients on the transplant waitlist by prioritizing those with the most pressing needs. In a recent study in Circulation, researchers at Children’s Hospital of Philadelphia (CHOP) reviewed the outcomes and found some patient groups benefitted from the allocation updates, while others did not experience the same level of improvement.
To assess how allocation policy changes affected heart transplant waitlist outcomes, researchers analyzed data from the United Network of Organ Sharing (UNOS) database. They identified 11,637 pediatric and adult patients with congenital heart defects or cardiomyopathy listed for transplantation. Patients were grouped by their type of cardiac disease and their listing status before or after key policy changes, with survival rates and waitlist removals due to clinical deterioration compared across different time periods.
Researchers found that children born with congenital heart defects experienced better outcomes after the 2016 changes. They were less likely to die or be removed from the transplant waitlist within a year of being listed. This improvement may be linked to advances in medical technology, such as increased use of mechanical heart support devices, allowing them to survive longer while waiting for a donor heart.
Adults with cardiomyopathy, a disease that weakens the heart muscle, also saw significant improvements after the 2018 policy changes. This group benefited from a revised system that prioritized those needing acute mechanical heart support, improving their access to life-saving transplants.
However, not all patients experienced the same success. Children with cardiomyopathy, for instance, did not see a noticeable reduction in waitlist mortality after policy changes. Likewise, adults with congenital heart defects did not show the same improvements as other patients.
The researchers noted that future updates of the allocation systems should take a few key points into consideration. Highlights include access to mechanical circulatory support options for children and adults with CHD, patient sensitization status (how likely a patient’s immune system is to reject a transplanted organ) and whether having separate systems for adults and children is the most appropriate method to allocate organs.
“Our findings underscore the importance of tailoring transplant policies to meet the unique needs of different patient groups,” said Jonathan B. Edelson, MD, an attending physician with the Division of Cardiology at Children’s Hospital of Philadelphia. “Recent allocation updates have introduced life-saving improvements, but further refinements are needed to ensure that all patients have equitable access to care, including potentially life-saving technology.”
The research was supported by a grant from the NIH (K23HL169833a).
Wooster et al. “Impact of Heart Transplant Allocation Changes on Waitlist Mortality and Clinical Practice in Pediatric and Adult Patients with Congenital Heart Disease and Cardiomyopathy.” Circulation. Online January 9, 2025. DOI: 10.1161/CIRCULATIONAHA.124.072335.
Featured in this article
Experts
Specialties & Programs
Heart transplant policies underwent significant changes in 2016 and 2018, altering how hearts are allocated to patients waiting for a transplant. These changes aimed to improve survival rates and outcomes for patients on the transplant waitlist by prioritizing those with the most pressing needs. In a recent study in Circulation, researchers at Children’s Hospital of Philadelphia (CHOP) reviewed the outcomes and found some patient groups benefitted from the allocation updates, while others did not experience the same level of improvement.
To assess how allocation policy changes affected heart transplant waitlist outcomes, researchers analyzed data from the United Network of Organ Sharing (UNOS) database. They identified 11,637 pediatric and adult patients with congenital heart defects or cardiomyopathy listed for transplantation. Patients were grouped by their type of cardiac disease and their listing status before or after key policy changes, with survival rates and waitlist removals due to clinical deterioration compared across different time periods.
Researchers found that children born with congenital heart defects experienced better outcomes after the 2016 changes. They were less likely to die or be removed from the transplant waitlist within a year of being listed. This improvement may be linked to advances in medical technology, such as increased use of mechanical heart support devices, allowing them to survive longer while waiting for a donor heart.
Adults with cardiomyopathy, a disease that weakens the heart muscle, also saw significant improvements after the 2018 policy changes. This group benefited from a revised system that prioritized those needing acute mechanical heart support, improving their access to life-saving transplants.
However, not all patients experienced the same success. Children with cardiomyopathy, for instance, did not see a noticeable reduction in waitlist mortality after policy changes. Likewise, adults with congenital heart defects did not show the same improvements as other patients.
The researchers noted that future updates of the allocation systems should take a few key points into consideration. Highlights include access to mechanical circulatory support options for children and adults with CHD, patient sensitization status (how likely a patient’s immune system is to reject a transplanted organ) and whether having separate systems for adults and children is the most appropriate method to allocate organs.
“Our findings underscore the importance of tailoring transplant policies to meet the unique needs of different patient groups,” said Jonathan B. Edelson, MD, an attending physician with the Division of Cardiology at Children’s Hospital of Philadelphia. “Recent allocation updates have introduced life-saving improvements, but further refinements are needed to ensure that all patients have equitable access to care, including potentially life-saving technology.”
The research was supported by a grant from the NIH (K23HL169833a).
Wooster et al. “Impact of Heart Transplant Allocation Changes on Waitlist Mortality and Clinical Practice in Pediatric and Adult Patients with Congenital Heart Disease and Cardiomyopathy.” Circulation. Online January 9, 2025. DOI: 10.1161/CIRCULATIONAHA.124.072335.
Recommended reading
A Lifesaving Fetal Heart Surgery
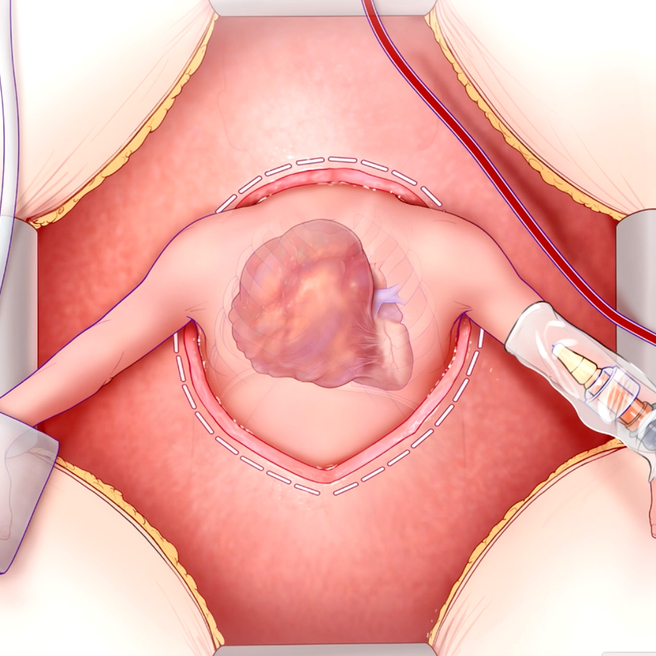
CHOP’s Center for Fetal Diagnosis and Treatment and Fetal Heart Program, successfully remove rare tumor from baby’s heart while still in the womb.
Contact us
Natalie Solimeo
Cardiac Center