Vaccine Science: Process of Vaccine Development
Initial ideas
Vaccine development typically begins not at a pharmaceutical company, but in a research laboratory in a university, medical center or small biotech company. Scientists in these laboratories are most often funded by grants from the government or private foundations. These scientists often spend years researching whether their ideas work, developing reagents and tests to measure their success (or lack thereof), and finally, using animals to test their ideas. In some cases the ideas are tested in small animals like mice, rats or rabbits and then again in larger animals like monkeys.
During this time, several different scientists or groups of scientists may be working toward the same goals: developing a vaccine against a certain virus or bacteria. The progress of these scientists is evaluated by other scientists through presentations at scientific meetings and peer-reviewed papers in journals. Scientists working at pharmaceutical companies often attend these meetings and review journals to see what ideas seem to be working. If any of the work seems promising, the pharmaceutical scientists may approach those working on it about expanding their research toward product development. This process may take five to 10 years.
The great majority of university scientists never develop ideas that are turned into products — most enjoy the success of adding to the general body of knowledge that is science.
Phase I trials
Once an idea appears promising, it must be tested in a small number of healthy adults. These placebo-controlled studies usually include less than 100 people and answer two main questions: does the vaccine generate the expected immune response and is the vaccine safe? (For more information about placebo controls, see "Phase III trials" section of page.)
During Phase I trials, scientists at the pharmaceutical company must study how to make the vaccine in a quantity large enough for preliminary trials. They also must determine what preservatives or stabilizers to add so that the vaccine does not break down and whether any adjuvants are necessary to generate a strong enough immune response. Any preservatives, stabilizers or adjuvants that are going to be in the final vaccine must be used in the trials.
In addition, company personnel must develop tests that consistently show positive results when expected and negative results when expected, and they must complete an application to inform the Food and Drug Administration (FDA) of their intentions.
This phase often takes one to two years to complete.
Phase II trials
The next phase of trials involves several hundred people, comparing those who did and did not receive vaccine (For more information about placebo-controlled trials, see "Phase III trials" section of page). During this phase, scientists try to determine the proper dose of vaccine to be given, and they continue to study the vaccine's safety. They also continue to define methods for manufacturing the vaccine, stabilizing the product, determining packaging vials, and establishing assays necessary for the trials. An important aspect of this phase is to establish manufacturing consistency, so that each lot comes out with similar results.
The manufacture of the vaccine must also be completed in the building that would be used to make the final product. The company must continue to keep the FDA apprised of its progress and results during this time. At any time during this process the company or the FDA can decide against continued development.
While Phase II trials can take as little as two years, it often takes much longer to complete all of the work necessary for this phase of development.
Phase III trials
This is the final stage of development before a company requests product licensing, and it takes three to four years to complete.
Studies in this phase of development include thousands of study participants who are similar to the population that will receive the vaccine (e.g., infants for a new infant product). The number of participants is calculated so that statistical differences between the experimental group and control group can be observed. These calculations depend on frequency of disease in the population, estimated participant dropout rates, and ability of the assays being used to show differences. For example, trials on the rotavirus vaccine (RotaTeq and Rotarix) required about 130,000 participants because the companies had to determine that these two vaccines did not cause a bowel obstruction caused by an older version of the vaccine (Rotashield).
During this phase, the company must also continue working on final facility and assay specifications and study how long the vaccine can be used before it expires, taking into account how it will get to the users (doctors' offices, for example) and how it will be stored. Any testing sites (those recruiting patients or testing samples) must be monitored to ensure that protocols are being followed consistently. Samples must be collected and analyzed to study the participants' immune responses, whether they get the disease, and whether they suffer adverse reactions.
During these studies, as with the previous phases, no one working with the patients, testing the samples collected from patients, or calculating the results, knows which participants received the vaccine and which did not.
After completion of these studies, it takes another year and a half to two years for the company to review the data, complete the product license request, and prepare to launch the product. The FDA, which does site visits throughout the entire process, then takes about 10 months to further study the data before the product can be offered to the public.
After licensure, experts for the Centers for Disease Control and Prevention (CDC) will also review the data and determine who should be able to get the vaccine. This is essentially the third set of scientists reviewing the same data. Often, the company or healthcare providers who helped run the Phase III studies will also publish the results in a scientific journal for review by other scientists.
By the time the product is offered to the public, it has been studied for at least 15 to 20 years (sometimes longer) in tens of thousands of study participants, by thousands of scientists, statisticians, healthcare providers and other personnel, and has cost at least $1 billion dollars to produce. There are many products that never reach this stage. Companies are constantly evaluating a product during the trials to determine whether they are worth pursuing. Many ideas are abandoned during the different trial phases.
Placebo-controlled vaccine trials
One of the important parts of the scientific enterprise is the inclusion of control groups. A control group is similar to the experimental group, except that it is not exposed to the experimental conditions. This allows scientists to determine the true effects of the experimental condition. As an example, when vaccines are tested in clinical trials, a control group similar to the vaccine recipient group in terms of age, health status and other factors will not receive the vaccine. Researchers will compare the results of the vaccine and control groups in terms of side effects, rates of infection, and more, allowing them to better understand whether the vaccine is safe and works.
The best type of study is a double-blind, placebo-controlled experiment, which means that neither the study subjects nor the researchers know who is in the experimental group and who is in the control group. Only after the code is broken can researchers determine who has received what. This is important because it prevents inadvertent biases from affecting the results. For example, if the experimental group knows they received the vaccine because they got a shot, they may have a greater tendency to report side effects than members of the control group who did not go through the experience of “getting vaccinated.” While some of what they report may, in fact, be the result of the vaccine, some of the reported side effects may simply be coincidental (e.g., a headache). On the other hand, if the control group knows they did not get the vaccine, they may not be as diligent about reporting what they are feeling (e.g., a headache). The result may be that unrelated “side effects” are attributed to the vaccine. In the example of headache, if the experimental group reports headaches and the control group dismisses them, the researchers may conclude that the vaccine causes headaches when, in fact, the results are simply because of how each group reported headaches. To prevent this from happening, control groups are often given placebos.
What is a placebo?
Placebos are designed to be similar to the experimental conditions, but they differ in that they do not include what is being tested. Placebos in vaccine trials can be a different vaccine, salt solution (called saline), or everything in the vaccine, except the part that will generate immunity, called the antigen.
By putting placebo doses in the same kind of vial with similar labeling to the experimental doses and coding both, the researchers giving the dose and the patients receiving it do not know whether it is vaccine or placebo. The people who prepare the doses and code them are different from those who administer them. In most studies, the code is not revealed until the trial is completed. On rare occasions, if a severe side effect is observed, the trial may be stopped and the code revealed to one or more senior investigators or statisticians to check whether the experimental doses are causing the effect. If they find that the severe side effects are occurring in those receiving the experimental doses, the trial will be stopped indefinitely, while scientists try to figure out what is happening. It may or may not be restarted.
Does it matter which type of placebo is used?
Some critics of vaccines, particularly those concerned about the effects of vaccine ingredients, promote the idea that vaccine trials do not use placebos, or that the placebos used in trials are inappropriate. In vaccine trials, appropriate placebos can include saline (a salt solution), diluent or culture medium (ingredients in the vaccine without the actual components of the pathogen), an existing vaccine that protects against the same pathogen, or other vaccines that would be given to the types of people in the trial. Whatever is used must be a logical choice to be able to detect any differences and be confident that they are the result of the vaccine being tested.
Find out more about the choice of placebo in this Unbiased Science Substack article.
Examples of placebo-controlled vaccine trials, sorted by vaccine
The following are examples of some vaccine studies that were completed for different vaccines and subsequently published in journal articles. This list is not exhaustive. The year represents the year the results were published, not the year the study was completed.
Cholera vaccine
- 1987: 1,257 participants; placebo: inactivated E. coli
- 2000: 17,799 participants; placebo: inactivated E. coli
- 1981: 237 participants; placebo: saline
- 1990: 114,000 participants; placebo: other childhood vaccines
Hepatitis A vaccine
- 1992: 1,037 participants; placebo: alum in vaccine diluent
- 1994: 40,119 participants; placebo: hepatitis B vaccine
- 2003: 274 participants; vaccine diluent
Hepatitis B vaccine
- 1980: 1,038 participants; placebo: alum in vaccine diluent
- 1982: 1,402 participants; placebo: alum in vaccine diluent
- 1982: 865 participants; placebo: alum in vaccine diluent
- 1983: 1,188 participants; placebo: human albumin and alum in vaccine diluent
- 1984: 1,311 participants; placebo: alum in vaccine diluent
Human papillomavirus (HPV) vaccine
- 2007: 5,455 participants; placebo: alum in vaccine diluent
- 2007: 12,167 participants; placebo: alum in vaccine diluent
- 2007: 18,644 participants; placebo: hepatitis A vaccine
- 2008: 7,466 participants; placebo: hepatitis A vaccine
Influenza vaccine
- 1985: 791 participants; placebo: saline or influenza type B vaccine
- 1994: 5,210 participants: placebo: saline or influenza type B vaccine
- 2006: 1,247 participants; placebo: saline
- 2008: 2,058 participants; placebo: saline or allantoic fluid
- 2009: 1,952 participants; placebo: saline
- 2011: 4,648 participants; placebo: saline
Meningococcal (ACWY) vaccine
- 2005: 1,398 participants; placebo: meningococcal polysaccharide vaccine
- 2009: 2,180 participants; placebo: previously licensed meningococcal vaccine (Menactra)
- 2016: 300 participants; placebo: TDaP (tetanus, diphtheria, acellular pertussis) vaccine
- 2018: 750 participants; placebo: other childhood vaccines
Meningococcal B vaccine
- 2014: 2,954 participants; placebo: Japanese encephalitis virus vaccine
- 2017: 2,968 participants; placebo: Japanese encephalitis virus vaccine
Mumps vaccine
- 1967: 867 participants; placebo: killed respiratory viruses
- 1967: 3,281 participants; placebo: saline
Pertussis (acellular) vaccine
- 1995: 1,942 participants; placebo: existing whole-cell pertussis vaccine
- 1996: 22,505 participants; placebo: DT (diphtheria and tetanus) vaccine
- 1997: 4,181 participants; placebo: existing whole-cell pertussis vaccine
Pneumococcal (conjugate) vaccine
- 2000: 37,868 participants; placebo: meningococcal vaccine
- 2000: 5,792 participants; placebo: meningococcal vaccine
- 2009: 12,031 participants; placebo: saline
Pneumococcal (polysaccharide) vaccine
- 1986: 2,295 participants; placebo: saline
- 2010: 1,006 participants; placebo: saline
Polio (inactivated) vaccine
- 1955: 455,474 participants; placebo: vaccine diluent
Rotavirus vaccine
- 1988: 104 participants; placebo: vaccine diluent and cherry syrup
- 1991: 321 participants; placebo: infant formula
- 1995: 898 participants; placebo: culture medium
- 1995: 325 participants; placebo: vaccine diluent and cherry syrup
- 1996: 1,216 participants; placebo: culture medium
- 1996: 700 participants; placebo: culture medium
- 1996: 540 participants; placebo: culture medium
- 1997: 2,207 participants; placebo: culture medium
- 1997: 1,185 participants; placebo: culture medium
- 1997: 2,398 participants; placebo: culture medium
- 2003: 731 participants; placebo: culture medium
- 2004: 439 participants; placebo: vaccine diluent
- 2006: 1,946 participants; placebo: vaccine diluent
- 2006: 68,038 participants; placebo: vaccine diluent
- 2006: 63,225 participants; placebo: vaccine diluent
- 2007: 3,994 participants; placebo: vaccine diluent
- 2008: 15,183 participants; placebo: vaccine diluent
- 2010: 5,468 participants; placebo: vaccine diluent
- 2010: 2,036 participants; placebo: vaccine diluent
- 2014: 4,532 participants; placebo: vaccine diluent
- 2014: 6,799 participants; placebo: vaccine diluent
- 2017: 3,508 participants; placebo: vaccine diluent
Typhoid fever vaccine
- 1980: 32,388 participants; placebo: vaccine preparation lacking active ingredient (antigen)
- 2001: 131,271 participants; placebo: saline
Varicella zoster (chickenpox) vaccine
- 1984: 956 participants; placebo: vaccine diluent
- 1996: 513 participants; placebo: vaccine diluent
Zoster (shingles) vaccine
- 2005: 38,546 participants; placebo: vaccine diluent
- 2012: 22,439 participants; placebo: vaccine diluent
Phase IV (after licensure)
Once the vaccine begins to be distributed, additional studies occur. These studies are called Phase IV studies. Because some rare side effects may not have been detected in the Phase III trials, vaccine safety is continually monitored by the CDC. These studies take at least four forms:
- First, the CDC will have certain health departments (usually in areas where there is a high occurrence of disease and hence, high vaccine distribution) monitor every person who receives the vaccine and report back regularly.
- Second, the CDC monitors diseases that are reported to every health department in the country, so they will see if there are any abnormal occurrences of disease after the vaccine is introduced and consider whether the two events may be related.
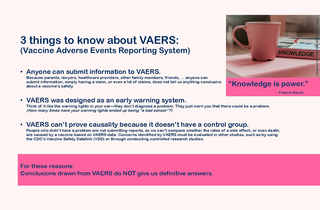
- Third, there is a Vaccine Adverse Event Reporting System (or VAERS). If a doctor, nurse or consumer believes that a person who received a vaccine had a significant negative side effect, he or she can file a report in this system, which is continuously monitored for trends in the data. Because this system does not take into account the number of doses of a vaccine that have been distributed, reports to this system cannot be used to determine whether a vaccine is causing a particular side effect. However, this system is critically important for the information it can provide to alert the CDC and the FDA of a potential issue. Once alerted, scientists and public health officials will quickly turn to other systems, like the Vaccine Safety DataLink, to analyze whether the issue is causally or coincidentally related to the vaccine.
View larger image:
- Fourth, the Vaccine Safety DataLink (VSD) includes about 6 million people in six large HMOs on the West Coast to look at who did and did not receive the vaccine and answer safety questions. The VSD is one of the most effective post-licensure measures we have.
These systems proved their utility in 1999 when a newly licensed rotavirus vaccine was found to be a rare cause of intussusception, a folding of the intestine into itself that may require emergency surgery and can result in death if untreated. Once the relationship was confirmed, use of that rotavirus vaccine was discontinued. A few years later, safer rotavirus vaccines were developed, and Phase III studies were of sufficient size to make sure these newer versions were not also causing intussusception.
Other info about vaccine development
Making sense of immunogenicity and efficacy data in vaccine trials
- Immunogenicity – a measure of the immune response generated after a person is vaccinated.
- Efficacy – a measure of the decrease in likelihood of getting infected with or developing a disease after being vaccinated.
Immunogenicity and efficacy may be used interchangeably in conversations about vaccination; however, they are not exactly the same thing. This is especially true when discussing or interpreting data from vaccine trials.
Immunogenicity usually comes first
Typically, the first clue as to whether a vaccine works is provided by measuring the immune response initially in experimental animals. Immunogenicity can be defined by any of the aspects of the immune response that are measurable. Most often for vaccines on the market, the measures are of antibodies in the blood, but in the research lab, measures can include newly formed or memory B cells, antibody secreting cells, or killer T cells to name a few. For some diseases, scientists know from previous work with the disease that if a person has a high enough level of one of these immune system components, he or she will be protected; this is called a correlate of protection.
Example: Someone with 15 international units (IU) of rubella-specific antibodies in the serum is considered to be protected against rubella. This is known as a correlate of protection.
If a correlate of protection is known and the potential vaccine does not induce a potent enough immune response, scientists need to reconsider the vaccine composition, dosage, and number and timing of doses. These studies can take years and are most often done in animals.
Unfortunately, for many diseases a clearly defined correlate of protection is not known. This is particularly true with infections that occur at mucosal surfaces (nose, throat, lungs, intestines and anogenital areas). In these cases, the most useful information comes from comparing the levels of the immune response following vaccination to those in individuals with disease.
- When measuring immunogenicity, typically the higher the numbers, the better the protection because they indicate a stronger immune response.
But does the vaccine work?
While immunogenicity is helpful in assessing whether a vaccine is likely to work, it does not completely answer the question about whether the vaccine actually does work. That is, will a person who got vaccinated be protected if he or she is exposed to the disease? Efficacy data provides this information. As with immunogenicity, when researchers measure efficacy, they can measure a few different things. Most often they look at mild, moderate and severe disease which identifies everyone who gets ill, but by classifying severity of disease, the findings provides additional information about how the vaccine works. In cases of mild or moderate disease, the vaccine worked by altering the course of disease, and likely prevented some deaths, so it could still be considered valuable.
- When measuring efficacy, less is more because the lower incidence of disease in vaccine recipients compared with unvaccinated people means the vaccine worked.
Revisiting immunogenicity
So, now you might be wondering why we still hear about immunogenicity data if efficacy data better defines how well a vaccine works. The answer is for a few reasons:
- Correlate of protection — If a correlate of protection is known for the disease, researchers can be confident that a vaccine candidate inducing an appropriate level of immunity will work, so they do not need to necessarily measure rates of disease.
- Ethics — It would be unethical to knowingly make someone sick just to see how well a vaccine works. Imagine giving some people an Ebola virus vaccine that we do not know works and then introducing Ebola virus into the community to compare the rate of vaccinated versus unvaccinated people who get ill. If the disease is common or the risk is high, such as polio in U.S. communities in the 1950s or currently, Ebola in parts of Africa, people who volunteer for a vaccine trial are taking a chance that it doesn’t work, but they are also increasing their chance to avoid the disease.
- Opportunity — After a vaccine is on the market, rates of disease typically decrease in a community, so comparing a newer version of a vaccine would be more difficult to do. In addition to being unethical —recipients might not be as well protected as if they got the vaccine that already exists —the chance of either group being exposed to the disease is smaller, so getting enough data to determine efficacy could prove arduous. However, researchers can compare the immunogenicity that develops after receipt of the new product with that of the existing product. If immunogenicity is similar between the two groups (new vaccine versus old vaccine), researchers can conclude that the new vaccine works. Further, if the new vaccine responses are low, they can still offer the superior product to those who were in the trial if it is deemed necessary for their protection.
Summary
Immunogenicity and efficacy data provide information on how well a vaccine works, but they are not the same. So, if you are reviewing or explaining data, it is important to determine how the study was designed and what it measured in order to appropriately interpret the data.
Reviewed by Paul A. Offit, MD on October 21, 2019