Tracheopexy
What is a tracheopexy?
A tracheopexy is a surgical procedure used to open and support the airway (windpipe) in severe tracheomalacia and some cases of recurrent tracheoesophageal fistula (TEF). In this procedure, a surgeon secures either the back wall of the windpipe to a strong ligament on top of the spine (posterior tracheopexy), or the front of the trachea to the breastbone/sternum (anterior tracheopexy). This prevents the trachea from collapsing. Air can then flow freely through the open airway.
Tracheopexy is a lasting solution for severe tracheomalacia. It is used to help children with severe collapse of the windpipe within the chest. The decision to recommend tracheopexy is made after all medical therapies have been tried and a child has been evaluated to determine the degree of tracheomalacia. In some cases, children with recurrent tracheoesophageal fistula may also be candidates for tracheopexy.
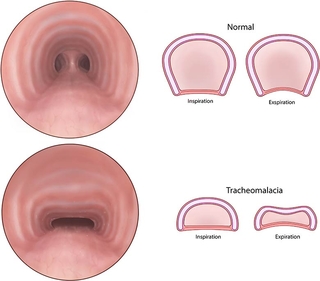
The images in the top row show a typical open windpipe and how it behaves when you inhale (inspiration) and exhale (expiration). The bottom shows a wider, flatter windpipe with tracheomalacia, and how the backwall can collapse even farther into the airway with forceful breathing or coughing (expiration).
Benefits of tracheopexy surgery
The benefits of the tracheopexy procedure can be significant. Studies have shown that posterior tracheopexy can effectively ease respiratory symptoms and lessen the degree of airway collapse in patients with severe tracheomalacia. This leads to fewer respiratory tract infections. In some cases, the procedure has allowed children to breathe freely and avoid the need for a tracheostomy, leading to a better quality of life.
The procedure does have risks. The tracheopexy surgery occurs near very important structures in the chest, including the heart, major blood vessels, windpipe and food pipe (esophagus). Because posterior tracheopexy moves the food pipe, a child may experience difficulty swallowing or dysphagia after surgery.
This is why it’s vital that this surgery be performed by an experienced team that fully understands a child's past medical history and anatomy.
Types of tracheopexy
There are two different approaches to tracheopexy: anterior and posterior. To help determine which type of tracheopexy to perform, our team will fully image the trachea to see the precise location of major blood vessels.
Posterior tracheopexy
A posterior tracheopexy is one approach to this procedure. While under general anesthesia, a skin opening, or incision, is made in the back side of the chest near the shoulder blade to reach the food pipe and windpipe.
First, the food pipe is moved away from any scar tissue in the chest and rotated to be side-by-side with the windpipe. This is called a “rotational esophagoplasty.”
If your child has a recurrent tracheoesophageal fistula (TEF), the connection (fistula) is located, and both the food pipe and windpipe are repaired during this stage.
With the food pipe side-by-side to the windpipe, sutures or stitches can be placed in the outermost layer of the windpipe at the area of tracheomalacia or airway collapse.
During this step, a pulmonologist is watching the inside of the windpipe with a bronchoscopy camera to be sure that no stitches come into the inside of the windpipe. These stitches are then placed into a strong ligament that is on the outside of the spinal bones. This holds the windpipe open during breathing and coughing. These stitches do not enter the spine and are very far from the spinal cord.
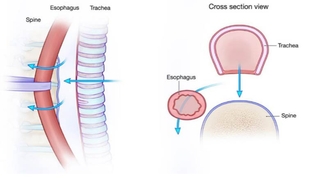
Usually, the esophagus (food pipe) is between the trachea (windpipe) and the spine. In this stage, the food pipe is rotated to the side of the windpipe to make room for the tracheopexy. Any recurrent tracheoesophageal fistula is repaired too.
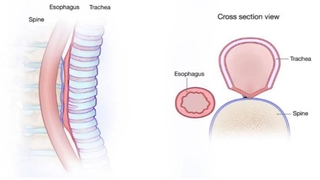
With the food pipe side-by-side to the windpipe, the outermost layer of the windpipe can be attached to the tough ligament on the outside of the spine to keep the airway open.
Anterior tracheopexy
An anterior tracheopexy is another approach to this procedure. Under general anesthesia, a skin opening, or incision, is made in the front of the chest over the breastbone (sternum). This bone is then opened (hemi-sternotomy) to gain access to the trachea from the front of the body and the major blood vessel coming from the heart, the aorta.
The outermost layers of the aorta and the trachea are carefully stitched and pulled forward and attached to the strong sternum. This keeps the airway open during breathing and coughing.
What to expect if tracheopexy is recommended for your child
Tracheopexy is a very specific surgery for very specific situations. Most children with tracheomalacia or airway collapse will thrive with nebulizers and careful follow up by a pulmonologist and will not need surgery.
When surgery is recommended, we do not rush the process. We take all the necessary steps to ensure a thoughtful and safe surgery.
Our surgical team is very large. It includes a team of nurses, nurse practitioners and physician assistants who will guide you through the process. Other team members include:
- General surgeons who specialize in airway surgery
- Otolaryngologists (ear, nose, and throat doctors)
- Pulmonologists (airway and lung doctors)
- Gastroenterologists (GI doctors)
- Speech and language pathologists
- Surgical dietitians
Usually, a breathing tube will be left in place after your child’s surgery. This allows us to provide strong pain medications and clean out secretions or mucous from the airway. This requires care in the intensive care unit (ICU) for the early part of recovery.
A chest tube will be placed during surgery to drain any fluids or air from your child’s chest. This is usually removed after your child resumes feedings after surgery.
Children will return to our clinic approximately three to six weeks after surgery for follow-up with the full team of specialists. They will assess breathing and coughing comfort, swallowing, nutrition, and overall healing.
Why choose CHOP for your child’s tracheopexy surgery?
Children's Hospital of Philadelphia (CHOP) is a leading choice for tracheopexy due to the exceptional experience and expertise of our surgical team. Our lead surgeon and lead gastroenterologist have a combined 25 years of experience in caring for patients with tracheomalacia, tracheoesophageal fistula and esophageal atresia. They have modified treatment techniques over time to improve patient outcomes.
Tracheopexy at CHOP is carefully guided by experienced pulmonologists who specialize in tracheomalacia. They take a thoughtful approach to referring patients for surgery, and they guide care before, during and after surgery.
This expertise and multidisciplinary approach ensures that patients receive the highest level of care and the best possible outcomes for tracheopexy procedures.