Pediatric ACL Reconstruction: Surgery to Repair a Torn ACL
What is ACL reconstruction surgery?
When the ACL (anterior cruciate ligament) is torn, the knee ligament will not heal on its own and surgery is needed to repair it. This procedure is called ACL reconstruction surgery.
In ACL reconstruction surgery, doctors remove the damaged ACL and replace it with new graft tissue.
ACL reconstruction surgery can use several different tissue grafts to replace the damaged ACL. Your child’s surgeon will discuss the best options available based on your child’s age, development and activity level.
Do you need surgery for a torn ACL?
For children, teens or young adults with complete or partial ACL tears, doctors will likely recommend ACL reconstruction surgery to repair the ligament. This will help your child resume an active lifestyle as soon as possible.
If the overall stability of your child’s knee is intact and they still have open growth plates, doctors may recommend non-surgical treatment.
When is ACL surgery recommended?
ACL reconstruction surgery is recommended for:
- Older adolescents, young adults and adults who have finished growing and no longer have open growth plates
- Individuals who have sustained a partial ACL tear (grade 2 injury) or complete ACL tear (grade 3 injury)
- Individuals who want to continue taking part in competitive sports that require cutting and twisting (i.e., football, soccer, basketball)
In most cases, ACL reconstruction is not recommended immediately following an injury. Instead, orthopedic surgeons typically prefer to wait until swelling has decreased and joint motion has returned. If an ACL reconstruction is performed too early, there is a significantly increased risk of scar tissue forming in the joint (called arthrofibrosis), which can lead to stiffness and loss of knee motion.
The importance of growth plates
Treatment for children and teens with ACL injuries is different than for adults. Youth are still growing and the ends of their bones – known as growth plates – are still developing. These partially formed bones are more sensitive to injury and can affect a child’s long-term growth. This adds an additional layer of complexity to ACL surgery in children.
At Children’s Hospital of Philadelphia (CHOP), our ACL surgery experts use several growth-sparing surgical approaches to avoid harming the growth plates. We have been pioneers in perfecting ACL surgery in growing children for decades.
How does ACL reconstruction surgery work?
The ACL can be reconstructed in a variety of ways. In most cases, tissue from the child’s own body is used to replace the damaged ACL. Most surgeries are minimally invasive, meaning no large incisions are needed. Instead, the surgeon will access the knee through several small ports and incisions.
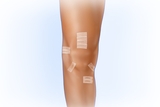
Fig. 1
Most ACL surgeries can be completed with five small incisions.

Fig. 2
The replacement tissue graft is passed diagonally through small tunnels in the thigh and shin bones and secured in place.
Tissue grafts used in pediatric ACL surgeries include the following. Pediatric surgeons always pay special attention to avoid damage to the growth plates.
A quadriceps tendon autograft
This procedure can be used for children with who are still growing and for teens who are fully grown. The ACL surgeon takes the central portion of the quad tendon (located between the kneecap and thigh), reinforces it with high strength suture, passes it diagonally through small tunnels in the thigh and shin bones, and then secures the graft in place with a button anchor.
This graft is:
- Stronger than the native ACL
- Does not remove muscle so patients can regain their strength
- Can be successfully used in techniques that respect both the growth plates and soft tissue in adolescent athletes, and in patients with closed growth plates
A patellar tendon autograft
This graft is sometimes used in older adolescents and in adults with closed growth plates. The surgeon removes a part of the patellar tendon (between the kneecap and shin bone) and a small amount of bone from the kneecap and shin bone. The graft is secured with anchors and/or buttons.
An iliotibial band autograft
This graft is used more commonly to address the ACL in pre-pubescent patients. The procedure involves removing a piece of the iliotibial band – or IT band – which runs along the outer part of the thigh. This graft also may be used for patients younger or older who have injured an additional ligament located between the outer side and the front of the knee.
Other options
In select cases, we may use the hamstring (located on the back of the thigh) as the graft. When tissue from the child’s body is not appropriate or available to be used as a graft, donor tissue – called an allograft tissue transplant – may be used.
Each tissue graft has advantages and disadvantages. Talk to your child’s orthopedic surgeon to decide which choice is best for your child.
ACL surgery recovery
During your recovery from ACL surgery, you’ll work closely with your surgeons and physical therapy team.
Rehabilitation after ACL surgery will initially focus on returning motion to the knee and leg muscles. Next, your child will work to make the new ligament stronger by slowly adding more pressure to it. Finally, your child will participate in a customized program designed to optimize return to their chosen sport or activities.
How long does it take to recover from ACL surgery?
Regrowth of the ACL takes time. It’s important to help your child have realistic expectations about their recovery. It could take 6-9 months or more for an athlete to return to sports after surgery, and a return to peak competitive performance may take upwards of a year.
Learn more about a typical path for ACL rehabilitation at CHOP.
Why choose CHOP for ACL reconstruction surgery?
Children are not tiny adults. Their bones, joints, tendons and ligaments are still growing and need individualized care from pediatric specialists who are most familiar with the unique needs of children and teens.
At Children’s Hospital of Philadelphia (CHOP), our Orthopedic Center and Sports Medicine and Performance Center offers:
- Volume and experience – We have one of the highest volume pediatric ACL programs in the world, drawing patients from across the United States and around the world.
- Customized care – We understand that every patient is different. Care must be individual to each patient’s age, size and development, along with any unique features of the tear (such as damage to the meniscus, ligaments and cartilage).
- Experience and precision – Surgery on young bones requires the utmost precision, and no one is more precise than pediatric surgeons who are used to working in very small spaces.
- Surgery techniques for young patients – CHOP is a world leader in growth-plate avoiding and growth-plate respecting techniques – having pioneered many of the techniques still in use. We also have led research in choosing and trialing ACL replacement tissues – many of which are stronger than the native ACL – and that decrease the chances of re-injury.
- A holistic focus on the young athlete – Our entire team (from surgeons to nurse practitioners, physical therapists and others) has experience evaluating the physical, mental and emotional needs of young athletes, from childhood to their young adult years. Patients, families and our team work together to make decisions about the best path forward for every individual patient.
Our goal for ACL treatment – no matter which path your family chooses – is to support your child and help them return to the activities they love.
Why choose CHOP for ACL repair
CHOP’s Sports Medicine and Performance Center is the region’s premier healthcare resource for youth athletes. We are nationally recognized for our surgical expertise and innovative treatments.
Safety in surgery
Our surgeons will always use the least invasive approach possible to repair an injury and help your child recover as quickly as possible.

What are the odds of tearing your ACL?
Understanding your risk of suffering an ACL tear is the first step to prevention. The CHOP team created an ACL risk analysis calculator to help estimate the yearly risk for a high-school athlete.