Patrick’s Story: Intravenous Immunoglobulin to Treat MOGAD
Patrick’s Story: Intravenous Immunoglobulin to Treat MOGAD
For Eileen and Brenden, March 14, 2020, is not only memorable because it was the day the United States declared a National Emergency due to the COVID-19 outbreak. It was also the day their son, Patrick, suffered a concussion that led to a potentially life-changing diagnosis.
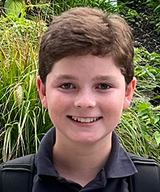
Patrick, 10, hit his head while playing kickball in his yard with some friends. After the injury, he complained that his head hurt and went inside his house to sit down. When Eileen checked on him, she found him muttering to himself as if in a trance.
Brenden called 911 and Patrick was rushed by ambulance to an emergency department (ED) near the family’s home in Wynnewood, Pa. There, Patrick was diagnosed with a concussion, observed briefly, and sent to the ED at CHOP for additional observation.
The physicians in the ED told Eileen and Brenden that it could take a few weeks for Patrick to fully recover from the concussion and connected them with a specialist. But nothing could prepare them for what happened next.
Diagnosing the underlying issue
Once home, Patrick often slept for 22 hours a day, had constant fevers and headaches, and vomited uncontrollably. After a few more visits to their local ED and an inpatient stay at that hospital — possibly due to the concussion, a flu diagnosis, or malnourishment related to the vomiting — the family arrived once again to CHOP’s ED. Patrick was now complaining of leg pain, in addition to all the other symptoms he’d been experiencing. He was examined by clinicians from neurology, ophthalmology, rheumatology and infectious diseases.
A magnetic resonance imaging (MRI) test revealed lesions in Patrick’s brain and spine. A subsequent blood test led to the diagnosis of myelin oligodendrocyte glycoprotein antibody disease (MOGAD), a disorder of the central nervous system that causes inflammation and potential damage in the optic nerve, spinal cord, brain and/or brainstem.
CHOP’s Neuroscience Center is a world leader in MOGAD research. Patrick was admitted to CHOP and underwent three days of therapy with intravenous corticosteroids, which alleviated his symptoms. When he hopped out of his hospital bed, tapped his mom on the shoulder, and asked her for a soft pretzel, she breathed a long-held sigh of relief. It had been weeks since her son had been interested in food.
Life with relapsing MOGAD

Before Patrick was discharged home, the team prepared the family for what to expect in the future. They explained that most patients respond well to intravenous steroids, that complete recovery from the initial MOGAD attack is common in about 70% of children, and in general the outcome is favorable. However, some patients relapse. MOGAD relapses can have long-term effects on the central nervous system, including gait and vision challenges.
Eileen, Brenden and the clinical team hoped Patrick would be among the 70% of kids who experience a complete recovery. But in the months that followed, Patrick periodically experienced problems with his vision. Each time, Eileen brought him back to CHOP and the clinical team found that new MOGAD lesions had formed.
In children with relapsing MOGAD, studies suggest use of intravenous immunoglobulin (IVIG) and/or disease modifying therapies. Patrick’s team created a therapy plan for him that involves IVIG every month for two years. Eileen says she was told Sarah Hopkins, MD, MSPH, a Pediatric Neurologist and Section Head for Neuroinflammatory Disorders at CHOP, would be the “quarterback” of Patrick’s robust care team, and she couldn’t have hoped for a better point person.
“She’s the one that I go to for absolutely everything,” says Eileen. “She’s very communicative, very approachable, super responsive. It’s so comforting to know that there’s a whole team of doctors who gather often to discuss Patrick’s case.”
Patrick, now 12, has wonderfully adapted to his diagnosis. He loves sports like basketball and soccer and, while symptoms have interrupted his playing on occasion, he is resilient and gets right back to it.
While there is some evidence of injury to Patrick’s optic nerves, his vision and neurologic examinations have been completely normal. He is very vigilant about reporting symptoms to his CHOP team to ensure early treatment.
Eileen and Brenden know Patrick may experience relapses his whole life, but they remain optimistic. And they know that their son’s care is in the best hands no matter what the future holds.
“Our CHOP team is amazing,” says Eileen. “I say all the time, ‘Thank God we live so close to CHOP,’ because they are recognized for their knowledge of rare diseases, and this one in particular. It’s very comforting. If I lived in a small town somewhere in the middle of the country, how long would it have taken to come to this diagnosis?”