Hematology / Oncology Fellowship Program
Overview and Mission

The mission of the Hematology/Oncology Fellowship Program at Children’s Hospital of Philadelphia (CHOP) is to prepare our fellows for a successful academic career as leaders in pediatric hematology/oncology.
To achieve this goal, we aim to:
- Recruit motivated and diverse trainees.
- Provide exposure to a broad range of hematologic and oncologic diseases.
- Create autonomous, accomplished clinicians with a formal mentorship structure.
- Guide trainees in principles of basic, translational and/or clinical research.
- Provide opportunities for lifelong learning and teaching others.
- Cultivate personal and professional qualities that facilitate teamwork, leadership and balance in the lives of our trainees to maintain longevity in the field.
We aim to prepare all fellows to function as accomplished clinicians capable of diagnosing and treating any patient with a hematologic or oncologic disease. Given the large, diverse clinical programs and individualized mentoring structure, our graduating fellows are enabled to become outstanding clinicians as faculty. Our goal is to recruit promising physician-scientists and prepare them for successful careers that advance basic, translational and clinical research in our field. Our formal mentorship system, Scholarship Oversight Committee input, along with an annual research retreat and professional development sessions contribute to a supportive, rich research environment. We work to cultivate personal and professional qualities that facilitate multidisciplinary teamwork and academic leadership. Finally, we aim to create a comprehensive, flexible curriculum that delivers core clinical and scholarly/research training for all fellows and tailor clinical, research and professional development to the goals of each fellow. Fellows may apply for an instructor position for 1 to 2 years to extend their research training and function clinically as an attending physician in order to be more competitive for academic positions.
Fellow/Grad Testimonials

“The breadth and volume of the training I received at CHOP is unparalleled. By the time I had completed my heme/onc fellowship, I felt well equipped to handle any patient who came through the door.”
— Lena Winestone
“Being surrounded by such bright and inquisitive people during my time at CHOP has prepared me for practice in academic pediatric oncology in a way I didn’t realize during training. I came out of fellowship feeling competent in the care of complex patients and had the exposures and mentorship needed to start and grow a clinical/translational research group as a junior faculty member. I also continue to maintain relationships with mentors from my time at CHOP, and the network created at that time has been invaluable in my continued career growth.”
— Andrea Franson
“Really excellent training with fantastic mentors and wonderful co-fellows. A great team to be a part of!”
— Caroline Diorio
“I cannot imagine training anywhere else. I left feeling prepared to be an attending for both hematology and oncology patients and also had a solid foundation to build a career as a clinical informatician with experience in clinical research.”
— Charles Phillips
“CHOP heme-onc fellowship program will prepare you to practice anywhere around the world! And this is from a former fellow who now practices in Israel!”
— Liron Grossmann
“Fostered independence in procedures, knowledge and taking care of complex patients. Established us as confident, autonomous attendings in oncology and transplant.”
— Jason Freedman
“CHOP’s hematology/oncology fellowship program was one of the highlights of my academic training. Not only did I receive excellent clinical and research training, but I also formed lifelong friendships with fellows and mentors whom I’ve stayed in touch with despite moving 5,000 miles across the country and Pacific Ocean. My training at CHOP has provided me the foundation to be a confident clinician, and the continued opportunity to collaborate with experts in the field both nationally and internationally.”
— Stephanie Si Lim
“I had the opportunity to be trained by nationally and internationally known pediatric oncologists. Their level of commitment to fellows always amazed me. They were always available to teach, mentor and support us. I am thankful the program supports firsthand learning side by side with radiology, path, genetics, cardiology, etc. Lastly, the program is very invested in constantly making itself better every year. There is a very collegial atmosphere. From someone who is close to her family, being able to develop those connections with co-fellows across all years & attendings was priceless. They truly became my family away from home.”
— Claudia Zapata
“I am grateful to have completed my peds heme/onc/BMT fellowship training at CHOP. The depth and breadth of my clinical training and limitless research opportunities is truly unique and incomparable.”
— Mike Leibowitz
Fellowship Leadership
Leslie Kersun, MD, MSCE, MSEd
Fellowship Director
Division Of Oncology - CHOP
Michael Hogarty, MD
Associate Fellowship Director
Division Of Oncology - CHOP
Alexandra Welch, BS
Hematology/ Oncology Fellowship Program Coordinator
Division Of Oncology - CHOP
Char Witmer, MD, MSCE
Clinical Director
Division Of Hematology - CHOP
Alexis Thompson, MD, MPH
Chief
Division Of Hematology - CHOP
Stephen Hunger, MD
Chief
Division Of Oncology - CHOP
Our Fellows
Class of 2024
Nora Gibson, MD
Residency:UCLA Mattel Children's Hospital
Medical School:University of Connecticut School of Medicine
Naomi Gunawardena, MD
Residency:UPMC Children's Hospital of Pittsburgh
Medical School:University of Pittsburgh School of Medicine
Saarah Hussain, MD
Residency:Children’s Hospital of Philadelphia
Medical School:Drexel University College of Medicine
Linah Omer, MD
Residency:Texas Tech University Health and Science Center
Medical School:Univ. of Khartoum Faculty of Medicine Sudan
Tim Spear, MD
Residency:Children’s Hospital of Philadelphia
Medical School:Loyola University Chicago Stritch School of Medicine
Daniel Zheng, MD
Residency:Boston Children's Hospital/Boston Medical Center
Medical School:Yale School of Medicine
Class of 2025
Jeremy Grenier, MD, PhD
Residency:Children’s Hospital of Philadelphia
Medical School:University of Connecticut School of Medicine
Andrew Hughes, MD, PhD
Residency:Children’s Hospital of Philadelphia
Medical School:University of Pittsburgh School of Medicine
Rachel Hurley, MD, PhD
Residency:Children’s Hospital of Philadelphia
Medical School:Mayo Clinic Alix School of Medicine
Aeesha Ranavaya, MD
Residency:Cincinnati Children's Hospital Medical Center
Medical School:Marshall University Joan C. Edwards School of Medicine
Mike Vido, MD, PhD
Residency:Children’s Hospital of Philadelphia
Medical School:Sidney Kimmel Medical College at Thomas Jefferson University
Adeline Yang, MD, MS
Residency:University of Texas Southwestern Medical Center
Medical School:University of Cincinnati College of Medicine
Class of 2026
Zach Berlant, MD
Residency:New York-Presbyterian (Columbia Campus) - Morgan Stanley Children’s Hospital
Medical School:Rutgers, Robert Wood Johnson Medical School
Abigail Berry, MD
Residency:University of Texas Southwestern
Medical School:University of Missouri-Columbia School of Medicine
Alexis Boulter, MD
Residency:University of Texas at Southwestern
Medical School:University of Florida College of Medicine
Alberto Guerra, MD, PhD
Residency:Boston Combined Residency Program (Boston Children's Hospital/Boston Medical Center)
Medical School:Perelman School of Medicine at the University of Pennsylvania
Ben Philipson, MD, PhD
Residency:Children’s Hospital of Philadelphia
Medical School:Perelman School of Medicine at the University of Pennsylvania
Monica Pomaville, MD
Residency:University of Chicago
Medical School:Michigan State University College of Human Medicine - Flint
How to Apply
We encourage you to apply through the Association of American Medical Colleges (AAMC) Electronic Residency Application System (ERAS) in July. We participate in the National Resident Matching Program (NRMP) with their usual timeline of Match Day in late November.
Clinical Training

The breadth and depth of clinical training is unparalleled. Fellows have a focus on the inpatient clinical care of patients with hematologic and oncologic diseases during year 1. They rotate at least twice throughout the sections of Oncology (Hematologic Malignancies, Solid Tumor, Neuro-Oncology and Blood and Marrow Transplant) and Hematology (Hematology Inpatient and Hematology Consult). Additionally, our fellows take inpatient call on hematology or oncology and serve as the point person for front-line providers on our units, staff in the Emergency Department or ICU, patients/families calling with questions, outside providers and our transport team.
Starting in year 1, fellows have both a hematology and oncology outpatient clinic where they follow a panel of patients and serve as the primary provider. There is a robust mentorship program to serve as backup and help educate our fellows in the outpatient care of their patients. Each fellow has a primary hematology faculty member who oversees the care of their outpatients. Additionally, fellows have a mentor in Hematologic Malignancy, Solid Tumor and Neuro-Oncology who help to educate them about their oncology outpatient panel. Their outpatient clinics serve as a formative educational experience as they learn to function as the physician for these patients and over the training program become autonomous in this care. During years 2 to 3, our fellows move to every other week clinics in both hematology and oncology in order to focus more of their time on research pursuits while continuing to be the primary provider for their outpatient panels.
Block Schedule for Hematology/Oncology Fellowship First Year Block Diagram
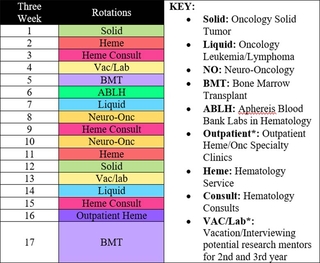
Fellows in years 2 and 3 don’t have any primary inpatient responsibilities. They continue to have on-call duties and have several weeks of night-float where they can condense more calls into a week and then have other weeks free for research activities.

Other clinical training for our fellows includes a mandatory “pretending” experience where third-year fellows serve as the attending for a week on the service of their choice. They work directly with a faculty member who orients them to the unique roles they may not have seen during training, gives feedback on their team leadership, clinical skills and teaching of residents/first-year fellows and allows them to feel autonomous running the inpatient team. Fellows gain procedural experience through our General Anesthesia (GA) clinic during the first year and may perform moderate sedation on their clinic patients for procedures in certain situations. Fellows return to GA clinic during their last year in order to review procedural skills. All fellows join our Blood and Marrow Transplant team for 2 to 3 bone marrow harvests during their training. Our first-year fellows also have an outpatient rotation where they gain exposure to some of the unique clinics and areas including radiation oncology, neurofibromatosis, survivorship and cellular therapy. Fellows also have a lab-based rotation during year 1 in order to learn about the Blood Bank, Coagulation Lab, Flow Cytometry, HLA/Immunogenetics, Anatomic Pathology and Hematopathology.

Research Training
Years 2 and 3 of fellowship (and year 4 if completing ARP training) are largely devoted to research (80%), with a reduced proportion of time allotted to clinical care. All types of research are valued: basic, translational and clinical. Within those domains, trainees work in diverse content areas: fundamental biology of hematologic and malignant disorders, drug and therapeutics development, outcomes, disparities, and health policy, among others. Many enter wet-labs and/or computational groups to pursue basic and translational research. Fellows interested in clinical research usually pursue a master’s degree to supplement their learning and these include the MSCE (Clinical Epidemiology and Biostatistics), MSHP (Health Policy), MSTR (Translational Research), MS in Bioethics and MS in Clinical Pharmacology.
All fellows create a tailored mentoring team to oversee their research training with programmatic input (Scholarly Oversight Committee). This includes a primary mentor and secondary mentors and advisors, both within and outside of the Divisions of Hematology and Oncology. We invite matched fellows to visit our campus in person or virtually prior to beginning their fellowship to meet with potential mentors, and we run an open campus for this purpose. Trainees can work with PIs within the Divisions of Hematology or Oncology at CHOP, outside of these divisions, or in laboratories at the University of Pennsylvania or the Wistar Institute. Those training outside of our divisions are required to have a mentor within the divisions to help oversee their professional development.

Throughout the research years we hold a monthly “Research Calls” curriculum. Year 1 calls (during the clinical year) review best practices for selecting a research pathway, project and mentor, and help clinical research-interested trainees prepare for MS program applications. The upper years calls focus on making a successful research transition, scholarship deliverables, and sharing experiences related to research training. This process is consolidated around a daylong Fall Research Retreat that addresses research topics: grant writing and submission basics, being a good mentor and a good mentee, and career development and professional transitions.
Our supportive environment, team mentoring, programmatic oversight, and vertical and horizontal peer mentoring are responsible for the tremendous successes of our trainees in securing competitive grants during fellowship and beyond.
Didactic and Other Educational Opportunities
There are a broad range of conferences and other educational opportunities for our fellows. First-year fellows on busy clinical services attend several conferences each week. Hematology Grand Rounds and POEM are required in addition to the clinical meeting of their current inpatient service. First-year fellows also attend Hematology School over the summer, Palliative Care Bootcamp in the fall and VitalTalk Communication Training Workshop in the early winter. On lighter rotations, they are encouraged to attend any other conferences of interest to them. For upper-level fellows, they have the required conferences as described for the first-year fellows and can attend monthly Marrow Transplant/Cellular Therapy didactics or any of the specialized hematology clinical conferences/journal clubs. They also have a yearly VitalTalk Communication Workshop to practice advanced skills and a monthly workshop in a variety of content areas including Comprehensive Vascular Anomalies, Gene Therapy for Hematologic Disorders, Relapsed Hematologic Malignancies and Bone Marrow Failure. Finally, there is a monthly professional development series with topics including bedside teaching, teaching around consults, giving feedback, faculty panels on career trajectory and work-life integration, quality improvement and financial planning.
Mentorship
We have a robust clinical mentorship program for each fellow. Fellows are assigned dedicated mentors in both hematology and oncology clinics. These faculty members see patients with the fellows weekly during the first year and then transition in the fall of the second year to every other week through the remainder of fellowship. Fellows are the primary physician for their patients, but the mentoring structure allows the fellows to have one faculty member (Hematology, Hematologic Malignancy, Solid Tumor, Neuro-Oncology) responsible for each of their patients throughout training. They know each patient and family well and serve at times as the behind-the-scenes helper to allow the fellows to cement longitudinal relationships with their patients/families. The clinical mentors are available at any time if questions arise about the fellow’s primary patients and help to see them when the fellow is on vacation or transitions to an every-other-week schedule during the upper years of fellowship. Over time, the clinical mentors give the fellows increasing autonomy to allow them independence in managing their outpatient clinical panels. Additionally, faculty serve as informal and/or life mentors to our fellows.
Research mentorship and Scholarship Oversight Committee
Wellness

Wellness is a significant priority of our training program. There are a variety of ways in which we work to support our fellows. We have one designated faculty member who is the wellness liaison to our Fellowship Committee and helps with ideas, programming and debriefing. Our fellow representatives help the leadership consider the impact of various activities and serve as our barometer for change. Examples of wellness initiatives include:
Supportive culture and building community:
- Budget for fellow class dinners, fellow-NP activities, fellow-faculty family-friendly activities
- Yearly graduation dinner for all faculty and fellows
- Welcome event for incoming fellows, current fellows and faculty
- Gatherings at national meetings
Debriefing and support:

First-year fellow debriefing with our wellness liaison
- Yearly all-fellow retreat off site with external facilitation
- Narrative medicine sessions run by the Cancer Center
- GME website with many helpful resources and local mental health providers. CHOP employees have access to the Employee Assistance Program which provides 6 to 8 appointments without charge.
- Challenging Interaction Tool allows fellows to report unprofessional behavior they witness or experience throughout the hospital. GME leadership is alerted and follows up with the reports on a regular basis.
Fellow input:
- Fellow representatives from second and third year serve on our committee, design the schedule, participate in feedback to leadership from retreat and national/local surveys
- Wellness liaison collates themes from debriefings to feed back to program leadership
Fellow recognition:
- Participation in Fellow Appreciation Week activities
- Quarterly fellow newsletter
- Recognition of our fellow representatives
Control over schedule:
- Fellow representatives design the schedule with input from program leadership
- First-year breaks from inpatient service: Outpatient rotation, time in the spring to catch up on clinical work, attend personal appointments and spend time in procedure clinic
- Night float system allows upper-level fellows to combine call in hematology and oncology to allow longer call-free periods in their schedule
Diversity, Equity & Inclusion
Hematology Diversity Committee
Led by Dr. Michele Lambert
Cancer Center Diversity Committee (CCDC)
Led by Drs. Cassie Kline and Lisa Wray
Mission Statement: Developing multipronged and multidisciplinary efforts to increase diversity and create an inclusive environment within the CHOP Cancer Center, ultimately reflecting diversity that mirrors the patients, families, and communities we serve. THIS WILL REQUIRE CULTURE CHANGE.
Committee Established: August 2019
Subcommittees Established: November 2020
- Education and Training
- Retention
- Hiring
Monthly Newsletters: Includes a spotlight of a Cancer Center member, vocabulary word of the month, holidays of the month, book of the month, video of the month, article of the month, holiday spotlights, educational information, DEI CHOP news, events, committee information, and resources.
Educational Opportunities for Employees: DEI Curriculum Series, Brave Space Series, unconscious bias training, liaison with MPN’s Mentorship Program, and DEI-related topics within the Narrative Medicine and Professional Development series sessions.
Educational Opportunities for Students: Commitment to a variety of pipeline programs ranging from PASS to CHOP RISES and beyond.
Events CCDC Hosts and Participates In: “Black Men in White Coats” documentary viewing and discussion, trivia nights, painting with a twist, wellness day, and back-to-school events.
CHOP-Wide Diversity Resources
Overview: Diversity Equity and Inclusion
Meet the Team: CHOP Office of Diversity, Equity & Inclusion Team
CHOP Employee Resource Groups
- AARG (All Abilities Resource Group)
- iSTEM (Inclusion in Science, Technology, Engineering and Math)
- LGBTQ+ Pride Resource Group
- MPN (Multicultural Professionals Network)
- US Military Resource Group
- Women’s Resource Group
- YPN (Young Professional Network)
CHOP Clinical Affinity Groups
- MPA (Multicultural Physician’s Alliance)
- AMP (Alliance of Minority Physicians)
- POP (Providers of Pride)
- MNA (Multicultural Nursing's Alliance)
Fellow Life
- Visit Philadelphia
- Visit Philadelphia - Philadelphia Neighborhoods
- CHOP Hematology/Oncology Fellows Instagram Page (handle is @chophemeoncfellows)
Salary/Benefits
Benefits and Compensation Resources for Residents/Fellows/T-32 Trainees >
Advanced Training Opportunities
Fellows have chosen a variety of advanced training opportunities after completion of our hematology/oncology fellowship. These include fellowships in palliative care and neuro-oncology. We have also had trainees who combined our fellowship with another training program such as clinical informatics.
Faculty Positions of Recent Fellows
Our fellows have been offered excellent opportunities for faculty positions after completion of training. We have former fellows at many outstanding academic institutions across the country and internationally.
Examples include:
- All Children’s Tampa
- Arnold Palmer/Orlando Health
- Baylor
- Children’s Healthcare of Atlanta
- Children’s Hospital of Philadelphia
- Denver Children’s Hospital
- Lurie Children’s Hospital
- Memorial Sloan Kettering Cancer Center
- New York University
- Penn State University
- University of Michigan
- Seattle Children’s Hospital
- Stanford University
- University of Chicago
- University of Hawaii
- University of Southern California
- University of California San Francisco
- Utah Children’s Hospital
Graduate Medical Education
CHOP is a national leader in training talented, diverse physicians who will shape the future of pediatric medicine. As the nation’s first pediatric hospital, we welcomed our first resident in 1873, and have since trained generations of experts in clinical care, research, advocacy and education. Learn more about Graduate Medical Education.