Patient Instructions: Low-Profile, Non-Balloon Gastrostomy Tube
These instructions are for Children’s Hospital of Philadelphia (CHOP) patients with a low-profile, non-balloon G tube (gastrostomy tube) for nutrition or medicine, also called a Bard® button or MiniOne® capsule button.
Important Information:
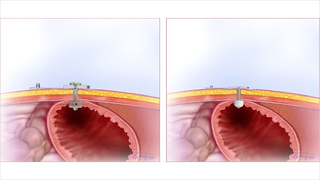
- Low-profile, non-balloon silicone gastrostomy tubes, also called button G tubes, have a mushroom-shaped bumper at the end. The mushroom bumper lies against the inside of the wall of the stomach.
- Low profile means that the part of the tube on the outside of the stomach lies flat against the skin of the belly.
- The mushroom-shaped bumper has a one-way valve that works like a trap door. When the valve is closed, nothing can pass through. To give feedings or medicines, a special tube called an extension set, is attached. The G tube also comes with decompression tubing to release air from the stomach. This is called venting.
- G tubes need to be changed routinely; your team will tell you how often.
- Your child’s tube should not affect normal activities. Your child can bathe, play, swim, and sleep as usual. This kind of tube works especially well for the active child because there is nothing hanging out to get caught on, and it is easily hidden under clothing.
Instructions for attaching and removing the extension set:
- Hold the button firmly with one hand.
- Open the safety plug on the button and insert the extension set completely, using a slight twisting action and pushing pressure.
- When a feeding is finished, flush the tube as you have been taught and remove the extension set with a slight twisting action and pulling pressure.
- Removing the extension set can prevent your child from pulling on the tube.
Instructions for cleaning the extension set:
- Wash the extension set in warm, soapy water after each use.
- Rinse well and hang to dry.
- Ask your homecare company how many sets you will be receiving each month so you know how often you can change them.
Instructions for skin care:
The stoma site is the opening where the G tube is inserted into the stomach. Wash around the stoma site and surrounding skin with mild soap and water every day, or more often if needed. Be gentle. Scrubbing can slow down healing or cause skin breakdown. Rinse with water and dry well. It is normal to have a little yellow-brown drainage and redness at the opening.
Call your child’s healthcare provider if you see:
- Rash with red dots on the edges
- Signs of infection: increased redness, swelling, yellow-green drainage with a bad smell at the stoma, pain
- Open areas of skin around the stoma
- Bleeding at the stoma site
- Bleeding, painful or growing granulation tissue around the stoma
- Increased leaking (formula or stomach fluid) at the stoma site
Instructions for leaking:
- Call your healthcare provider if the tube is leaking.
- While you are waiting to get instructions, keep your child’s skin dry by changing any wet gauze or dressing under the tube as needed.
- Protect the skin around the stoma with a skin barrier, such as Vaseline®, A & D® ointment, diaper cream, or Cavilon™ No Sting Barrier Film (if your child is over 1 month of age).
Instructions for treating granulation tissue:
Granulation tissue is a type of scar tissue that forms when the body is trying to heal itself. Because the feeding tube stoma is a new opening, your child’s body naturally may try to close it by growing this tissue. Some children have granulation tissue that grows very quickly, while others have no problem with it at all. Granulation tissue is dark pink or red. Sometimes it can cause leaking and skin irritation. It may also bleed or cause pain. If this happens contact your healthcare provider.
- If you see granulation tissue starting to grow, discuss it with your healthcare provider at your next visit.
- If the granulation tissue around the tube is bleeding, painful, or growing quickly, contact your healthcare provider for an appointment. They may prescribe a cream that you can use at home, or they may treat it in the office with a medicine called silver nitrate. These medicines shrink the granulation tissue. Granulation tissue may return and need to be treated with medicine again.
Instructions for venting the G tube:
Venting is a way to use the tube to burp your child and let gas out of their stomach. Your child may need to be vented if their belly is bloated, if they have belly pain, or if they gag, retch, or vomit.
If your child’s tube needs to be vented, follow these steps:
- Place the decompression extension set into the button.
- Remove the plunger from a catheter tip syringe and attach the open barrel to the decompression extension set.
- Keep the tube vented for 5-10 minutes before and after feeding or as instructed.
- If this does not work, turn the decompression tube to open the valve.
Instructions if the G tube becomes clogged:
- Try to prevent the tube from clogging by flushing the tube with water as directed after each feeding and before and after each medicine. If your child is on continuous feedings, the tube needs to be flushed at least once a day.
- Even a tube that is not being used must be flushed once a day.
- If the tube becomes clogged, attach a 5 ml oral syringe with warm water to the end of your feeding tube extension set. Try to flush the tube. If you are unable to flush, pull back on the plunger of the syringe. Repeat this push and pull action up to 5 times. If you still cannot flush the tube, try using warm water in a 3 ml or 1 ml oral syringe and repeat the above steps.
- If this does not work, call your healthcare provider.
Instructions if the G tube comes out:
No matter how long your child has had a G tube, the stoma can close very quickly. If the G tube comes out and you are:
- If you are less than 45 minutes away from one of CHOP’s hospitals, go to the nearest CHOP Emergency Department in Philadelphia or King of Prussia.
- More than 45 minutes away from CHOP, go to the closest Emergency Department.
- If you go to another Emergency Department, ask them to call your child’s healthcare provider at CHOP.
Call your CHOP team with any questions or concerns.
If you have any questions about your child’s health, please contact your child’s healthcare provider. This document is intended only to provide general educational information and is not intended as medical advice or treatment. Please consult with your healthcare provider prior to use, as some of this information may need to be adapted for your child’s specific needs. It is the responsibility of your healthcare provider to advise you on the appropriate use of this information. If you/your child are not already a CHOP patient, this document does not create a doctor-patient relationship between you/your child and CHOP. CHOP is not responsible for any outcomes you/your child might experience from your use of this document. This document is provided "AS IS", WITHOUT WARRANTIES OR CONDITIONS OF ANY KIND, express or implied. If this document refers to any drugs or medical devices, it is the responsibility of your healthcare provider to check the FDA status prior to use. If this document includes references to drug dosing, please do not rely on this document. Your healthcare provider should check the package insert for each drug before use. Hyperlinks used within this document may not be translated into other languages.
©2022 Children’s Hospital of Philadelphia. Not to be copied or distributed without permission.