Patient Instructions: Gastrostomy Tube or Gastro-Jejunostomy Tube placed by Interventional Radiology
These instructions are for Children’s Hospital of Philadelphia (CHOP) patients with a G tube (gastrostomy) or GJ tube (gastro-jejunostomy), also called a Corpak® or Corpak with Corflo J tube®, placed by Interventional Radiology.
Important information:
- A gastrostomy tube, also called a G tube, is threaded through the mouth, down the food pipe (esophagus), and exits from the stomach. The opening on the skin that the tube goes through is called a stoma. The tract is the pathway leading from the stoma into the stomach. After about 6 weeks or more the tract should be healed, and your child may receive a different type of tube called a low-profile button tube.
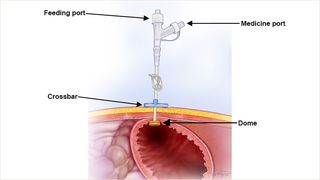
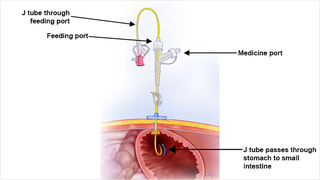
- Your child’s tube has a small dome inside the stomach that you cannot see, to hold it in place. It also has a crossbar on the outside that rests against the belly to help hold it in place. The tube sits outside the belly, about 8-10 inches. The tube has 2 openings that are used to give feedings and medicine.
- Sometimes another smaller feeding tube is threaded through one of the openings and passes through the stomach and into your child’s small intestine (jejunum). This is called a GJ tube, or gastrojejunostomy tube. This type of tube is used for children who cannot have feedings into their stomach.
Instructions for care of the tube:
It is important to secure the tube to prevent it from coming out and to prevent the tube from moving so the stoma and tract can heal. Poor healing can cause fluid to leak from the stomach, skin irritation, and skin breakdown.
Tips to keep the tube from moving:
- Keep the bumper up against the wall of the stomach and the crossbar resting on the skin. Note the number on the tube next to the crossbar. This tells you the tube has not moved.
- You may tuck the tube into your child’s clothing, but not near their diaper area.
- ElastiNet®, a stretchy elastic net dressing, may also be used to keep the tube close to your child’s body.
- Your child’s tube should not interfere with their normal activities. They can play and sleep as usual. Clothing such as onesies, one-piece outfits, and “bib” type outfits may prevent your child from pulling on the tube. This type of clothing can also prevent the tube from getting caught on something and keep it from getting pulled out.
- The tube may be taped so that it does not move out of place. If the tape becomes loose, do not remove it. Reinforce it with more tape and call Interventional Radiology.
Instructions for skin care:
- The gauze dressing around a newly placed tube is removed after 24 hours, and a dressing is no longer needed.
- The site may be tender for a few days.
- For the first 2 days after surgery, your child can only have sponge baths. The G tube site should not go under water. After 2 days, your child may shower. Once 2 weeks have passed, they may take tub baths and swim.
- Wash around the stoma site and surrounding skin with mild soap and water every day, or more often if needed. Be gentle. Scrubbing can slow down healing or cause skin breakdown. Rinse with water and dry well. It is normal to have a little yellow-brown drainage and redness at the stoma.
- Turn the crossbar every 8 hours while your child is in the hospital. When you go home, turn the crossbar 2-3 times a day for 1 week. This prevents irritation and skin breakdown.
Call your child’s healthcare provider if you see:
- Rash with red dots on the edges
- Signs of infection: increased redness, swelling, yellow-green drainage with a bad smell at the stoma, pain
- Open areas of skin around the stoma
- Bleeding at the stoma site
- Bleeding, painful, or growing granulation tissue around the stoma
- Increased leaking at the stoma site
- Vomiting formula when on J tube feeds.
Instructions for leaking:
- Make sure the tube is secure with the bumper up against the wall of the stomach and the crossbar resting on the skin.
- If leaking continues, call Interventional Radiology.
- While you are waiting to get instructions from your healthcare provider, you may place a small piece of gauze or other dressing around the tube. Change it when wet.
- Protect the skin around the stoma with a skin barrier, such as Vaseline®, A & D® ointment, diaper cream, or Cavilon™ No Sting Barrier Film (if your child is over 1 month of age).
- If leaking is from the Y-port, change the Y-adaptor as you were taught.
Instructions for treating granulation tissue:
Granulation tissue is a type of scar tissue that forms when the body is trying to heal itself. Because the feeding tube stoma is a new opening, your child’s body naturally may try to close it by growing this tissue. Some children have granulation tissue that grows very quickly, while others have no problem with it at all. Granulation tissue is dark pink or red. Sometimes it can cause leakage and skin irritation. It may also bleed or cause pain. If this happens contact your healthcare provider.
- If you see granulation tissue starting to grow, discuss it with your healthcare provider at your next visit.
- If the granulation tissue around the tube is bleeding, painful, or growing quickly, contact your healthcare provider for an appointment. They may prescribe a cream that you can use at home, or they may treat it in the office with a medicine called silver nitrate. These medicines shrink the granulation tissue. Granulation tissue may return and need to be treated with medicine again.
Instructions for venting the tube:
J tubes do not need to be vented, but G tubes may need to be. Venting is a way to use the tube to burp your child and let gas out of their stomach. Your child may need to be vented if their belly is bloated, if they have belly pain, or if they gag, retch, or vomit.
If your child’s G tube needs to be vented, follow these steps:
- Remove the plunger from a catheter tip or oral syringe.
- Attach syringe barrel to tube.
- Hold syringe barrel above the level of your child’s stomach.
- Keep the tube vented for 5-10 minutes before and after feedings or as instructed.
Instructions for a clogged tube:
- Try to prevent the tube from clogging by flushing the G tube port with water or air as directed after each feeding and before and after all medications.
- If the G tube is not being used, it must be flushed once a day.
- The J tube can clog easily and needs to be flushed with 5-10ml of warm water every 2-4 hours throughout the day, after all feedings, and before and after all medicine.
- If either the G or J tube becomes clogged, attach a 5ml oral syringe with warm water to the end of your feeding tube. Try to flush the tube. If you cannot flush, pull back on the plunger of the syringe. Repeat this push and pull action up to 5 times. If you still cannot flush the tube, try using warm water in a 3ml or 1ml oral syringe and repeat the above steps.
- If you still cannot flush the J tube, use the Clog Zapper® kit as you were taught. Clog Zapper is a ready-to-use kit containing a powder that helps break up clogs in feeding tubes. Clog Zapper contains maltodextrin, a type of sugar. If your child is on a ketogenic diet, they will need microlipids once the tube is unclogged. Talk to your healthcare provider about how much to give. Clog Zapper also contains coconut and should not be used in those with tree nut allergies.
- Call Interventional Radiology if you cannot unclog the tube.
Instructions if the G tube or GJ tube comes out:
- No matter how long your child has had a G tube or GJ tube, the stoma can close very quickly. If the G tube or GJ tube comes out and you are:
- If you are less than 45 minutes away from one of CHOP’s hospitals, go to the nearest CHOP Emergency Department in Philadelphia or King of Prussia.
- More than 45 minutes away from CHOP, go to the closest Emergency Department.
- If you go to another Emergency Department, ask them to call Interventional Radiology at CHOP.
Call your CHOP team with any questions or concerns.
If you have any questions about your child’s health, please contact your child’s healthcare provider. This document is intended only to provide general educational information and is not intended as medical advice or treatment. Please consult with your healthcare provider prior to use, as some of this information may need to be adapted for your child’s specific needs. It is the responsibility of your healthcare provider to advise you on the appropriate use of this information. If you/your child are not already a CHOP patient, this document does not create a doctor-patient relationship between you/your child and CHOP. CHOP is not responsible for any outcomes you/your child might experience from your use of this document. This document is provided "AS IS", WITHOUT WARRANTIES OR CONDITIONS OF ANY KIND, express or implied. If this document refers to any drugs or medical devices, it is the responsibility of your healthcare provider to check the FDA status prior to use. If this document includes references to drug dosing, please do not rely on this document. Your healthcare provider should check the package insert for each drug before use. Hyperlinks used within this document may not be translated into other languages.
©2022 Children’s Hospital of Philadelphia. Not to be copied or distributed without permission.