Percutaneous Gastrostomy Tube Placement
What is a percutaneous feeding tube?
The term “percutaneous” means “to go through the skin.” A percutaneous feeding tube is placed through the abdominal wall into the stomach to allow feeding directly into the stomach or intestines. A feeding tube into the stomach is a gastrostomy tube, or G tube; a tube feeding into the intestines is a gastrojejunostomy tube, or GJ tube.
Will my child be awake during the procedure?
No. The procedure will be performed with IV sedation or general anesthesia.
Learn more about sedation and anesthesia.
Will my child be in any pain?
Your child may experience discomfort around the tube for several days. We will give your child pain medicine to alleviate the tenderness.
How long does the procedure take?
Generally the procedure takes one hour. However, it may take longer.
What risks are associated with this procedure?
This procedure is considered low risk. However, complications may occur, including:
- Tenderness or soreness at the site where the tube is placed
- Bleeding
- Infection
- Injury to the esophagus, liver, spleen, colon or other organs, which may require additional procedures and/or surgery to repair
- Peritonitis, a serious condition in which the lining of the abdominal cavity becomes inflamed
What will happen during the procedure?
We begin by examining your child’s upper abdomen with an ultrasound probe, to locate the liver and spleen. We insert X-ray dye (contrast) through the rectum into the colon, and pass a small tube through your child’s nose into the stomach and inject some air into the stomach. These steps allow us to identify important structures in the abdomen, so we can choose a safe place for the feeding tube.
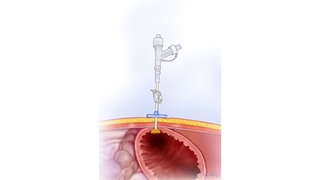
Once we have marked a spot for the feeding tube, we will inject a local numbing medicine into the skin. The interventional radiologist will use live X-ray (fluoroscopy) to guide the passage of a needle through the skin into the stomach. (Your child will be protected by an X-ray shield.) Then, using a special technique, the doctor will guide the tube through your child’s mouth, down the esophagus, into the stomach, and then out of the stomach through a small incision (approximately 1 centimeter).
Very rarely, patients experience airway compromise, which means they have difficulty breathing while the tube is passed through the esophagus. We will monitor the level of oxygen in your child’s blood throughout the procedure. If airway compromise occurs, we will know immediately and correct it.
What happens after the procedure?
Your child will be admitted to the hospital for an overnight stay. We will give your child pain medicine and antibiotics to reduce the risk of infection. Your child will probably have some pain or mild discomfort around the tube for several days.
We will begin feeding your child through the tube eight hours after the procedure as long as there are no symptoms. We will teach you how to care for your child’s feeding tube. Your child won’t have any stitches at the site of the tube. There will be a small piece of gauze between the tube and the skin.
Your child will have a follow-up appointment with Interventional Radiology 10 days after the procedure to inspect the site.
When can my child bathe?
Your child may shower or take a sponge bath 48 hours after the procedure. It is very important that the area around the tube is not submerged in water for two weeks.
Are there any activity restrictions?
There are no specific activity restrictions. However, your child shouldn’t participate in contact sports or rough playing that might pull the tube.
How long will the primary tube stay in place?
After three months the primary tube will be removed and changed to a low-profile button, which sits 1 to 2 centimeters off the skin, or another type of tube called a long, floppy tube, which hangs out approximately 6 inches. Your referring physician will decide which type of tube is best for your child.
These tubes are inserted and removed more easily than the original. They will be changed every three months on an outpatient basis without sedation.