What is spina bifida?
Spina bifida is a birth defect in which an area of the spinal column doesn’t form properly, leaving a section of the spinal cord and spinal nerves exposed through an opening in the back.
Spina bifida occurs in 1 per 2,000 live births in the United States and is the most common central nervous system birth defect. Around 1,500 babies are born with spina bifida in the U.S. each year. Find some more fast facts about spina bifida.
Myelomeningocele

The most common and serious form of spina bifida is called myelomeningocele (my•e•lo•me•nin•go•cele) (MMC), in which part of the spinal cord and surrounding nerves push through the open bones (vertebrae) in the spine and protrude from the fetus’ back.
Usually, the exposed spinal cord and nerves are contained in a sac that is exposed to amniotic fluid. Continuous bathing of the fragile developing spinal cord in amniotic fluid over the course of gestation is thought to result in progressive neurologic injury. Until recently, spina bifida treatment was relegated to post-birth surgery after damage from continuous exposure to amniotic fluid was already made.
Other types of spina bifida
Other types of spina bifida include myeloschisis, lipomeningocele and myelocystocele. Open neural tube defects such as myelomeningocele and myeloschisis are treatable by fetal repair. Closed neural tube defects such as lipomeningocele and myelocystocele are not treatable by fetal repair.
Causes of spina bifida
Myelomeningocele has genetic and micronutrient causes. Mothers who have had a baby with spina bifida have up to a 4 percent risk of recurrence in subsequent pregnancies.
Spina bifida symptoms
The myelomeningocele lesion can occur at any level on the developing spine, but most are found in the lumbo-sacral region. Depending on the lesion’s location, myelomeningocele may cause:
- Bladder and bowel problems (incontinence)
- Sexual dysfunction
- Weakness and loss of sensation below the defect
- Inability to move the lower legs (paralysis) and other cognitive impairments
- Orthopedic malformations such as club feet or problems of the knees or hips
Generally, the higher the defect is located on the spine, the more severe the complications.
In many cases, the brain develops an Arnold-Chiari II malformation, in which the hindbrain herniates or descends into the upper portion of the spinal canal in the neck. This herniation of the hindbrain blocks the circulation of cerebrospinal fluid, causing hydrocephalus (accumulation of fluid in the brain), which can injure the developing brain. Ventricular shunting (placement of a thin tube into the ventricles of the brain) is used to drain fluid and relieve hydrocephalus.
Spina bifida can lead to a variety of social and emotional challenges and lifelong quality-of-life issues.
Evaluation and diagnosis of spina bifida
As with other birth defects, most myelomeningoceles are discovered by routine ultrasound evaluation between 16 and 18 weeks into the pregnancy.
Sonographic features suggestive of myelomeningocele include a cystic mass anywhere on the spine. If no skin covers the defect, abnormally high alpha-fetoprotein (AFP) levels in the blood and amniotic fluid will support the diagnosis.
Mothers referred to CHOP’s Center for Fetal Diagnosis & Treatment for a spina bifida diagnosis undergo a comprehensive, one-day evaluation that includes:
- High-resolution level II ultrasound — to confirm the diagnosis and determine the location of the lesion, and to assess for any other birth defects such as club feet
- Ultrafast fetal MRI — to confirm presence of the Chiari II malformation and to screen for evidence of any other neurologic abnormalities
- Fetal echocardiogram — to determine any problems with the heart
- Amniocentesis — to confirm the presence of elevated amniotic fluid alpha-fetoprotein (AFAFP) levels and acetylcholinesterase (AChE), which indicate open neural tube defects
Fetal MRI showing a fetus with spina bifida Maternal serum alpha-fetoprotein (MSAFP) test — to confirm elevated AFP levels in the mother’s blood
After evaluation, you will meet with our multidisciplinary team, including a fetal surgeon, a neurosurgeon, an anesthesiologist, a maternal-fetal medicine specialist and a coordinator. The purpose of this meeting is to review your test results, confirm the diagnosis, explain spina bifida treatment options and potential outcomes, and answer all of your questions.
Delivery of babies with spina bifida
Delivery for all babies with myelomeningocele takes place in CHOP’s Garbose Family Special Delivery Unit (SDU), allowing for the highest level of immediate care for the newborn, as well as expert obstetric services for the mother — all within a leading pediatric hospital. The world’s first birth facility designed exclusively for pregnancies complicated by birth defects, the SDU is a vital part of our team’s ability to provide comprehensive care for spina bifida.
Spina bifida treatment
The two main spina bifida treatment options are fetal surgery during pregnancy or surgery on the baby right after birth.
Deciding whether prenatal or postnatal spina bifida repair is appropriate is influenced by several considerations, including gestational age, the level of the myelomeningocele lesion on the spine, presence of the Chiari II malformation, and a number of important maternal health factors.
Prenatal repair also requires a significant commitment on the part of the mother and her support person. Read our criteria for fetal surgery to determine when fetal surgery for myelomeningocele is an option.
Our team helps each family fully understand the benefits and risks of spina bifida treatment so they can make the best decision for their unique situation. Our team also counsels and supports families who choose to terminate the pregnancy.
Watch this video to learn more about spina bifida treatment options, the benefits of spina bifida surgery before birth, and the support services CHOP offers families.
Where to start when you learn your baby has spina bifida
For parents who find out their unborn baby has spina bifida, the biggest question is often “what do I do next?” Here’s advice on where to start.
MMC fetal surgery outcomes
Learn about key outcomes and measures of success in fetal repair of spina bifida and see how CHOP's experience compares.
Spina bifida surgery after birth
If postnatal spina bifida surgery is recommended or selected, your pregnancy is monitored — often at your home hospital — and a cesarean delivery is planned at CHOP at 37 weeks.
Traditional spina bifida treatment takes the form of surgical repair 24 to 48 hours after birth. Your child will undergo general anesthesia. A pediatric neurosurgeon removes the MMC sac, if one is present, and closes the surrounding tissue and skin over the defect to protect the spinal cord. After surgery, your baby will receive care in our Newborn/Infant Intensive Care Unit (N/IICU).
Spina bifida surgery before birth
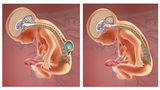
Because spinal cord damage is progressive during gestation, prenatal repair of myelomeningocele may prevent further damage.
Experts at Children’s Hospital of Philadelphia (CHOP) co-led the landmark Management of Myelomeningocele Study (MOMS), which compared outcomes after prenatal and postnatal repair of myelomeningocele. Results demonstrated that prenatal repair can offer significantly better results than traditional postnatal repair:
- Reduced the need to divert fluid from the brain using ventricular shunting
- Reduced the incidence or severity of neurological effects such as impaired motor and sensory function of the legs
- Improved mobility and improved the chances that a child will be able to walk independently (see report confirming improved motor outcomes at 30 months)
- Reversed the hindbrain herniation component of the Arnold-Chiari II malformation
In a follow-up study 10 years later (MOMS2), new findings showed significant physical and emotional benefits in school-age children who received corrective surgery in the womb for MMC. Researchers continue to follow families involved in the study to measure longer term outcomes in their patients. The next phase of the study, known as MOMS3, is now following children up to ages 15 to 24, and will build upon the research in MOMS and MOMS2.
Fetal surgery for spina bifida is a complex and challenging procedure, requiring the most expert, comprehensive care for both mother and fetus. The surgical team’s level of experience and all aspects of care surrounding the operation are of paramount importance. See a report on key outcomes and measures of success reported by our team since the MOMS trial to learn more about our experience and results.
If your unborn baby has been diagnosed with myelomeningocele and you are a candidate for prenatal spina bifida treatment at Children’s Hospital of Philadelphia, the surgery is performed between 23 weeks and 25 weeks 6 days gestation.
Fetal surgery for myelomeningocele (MMC), the most severe form of spina bifida, is offered as a standard of care at CHOP.

Spina bifida prognosis
Rarely children can pass away due to complications associated with Chiari II malformation or hydrocephalus. Many patients require shunts (85 percent), and 45 percent of shunts develop complications within one year.
Follow-up care
Children’s Hospital provides comprehensive long-term follow-up for children with spina bifida, from the time of repair through adolescence. Our dedicated Spina Bifida Program’s interdisciplinary team includes a pediatrician, nurse, social worker, physical therapist, neurosurgeon, orthopedic specialists, urologist and genetic counselor — all focused on the care of children with spina bifida. As needed, other subspecialists within CHOP are consulted.
Follow-up includes visits every four to six months until age 2, then annually, with urodynamic testing and renal bladder ultrasounds to ensure kidneys function properly and bladder function is stable.
Depending on the location of the lesion and outcome after surgery, follow-up care may also include:
- Clean intermittent catheterization
- Bowel management
- Lower extremity bracing
- Physical therapy evaluation and guidance to outside physical therapists and early intervention
- Pressure sore management
- Referral to appropriate psychosocial and financial resources
- Consultation with other subspecialties including ophthalmology, nephrology, nutrition and feeding specialists, and plastic surgery
The Spina Bifida team works closely with each child’s primary care pediatrician and school, and helps families access appropriate community services.
Ongoing follow-up is critical when it comes to improving outcomes and advancing treatment for patients with myelomeningocele.

Why Choose Us
At the Wood Center for Fetal Diagnosis and Treatment, you and your baby are in the hands of one of the most experienced fetal programs in the world.

Tour our Fetal Center
The Wood Center for Fetal Diagnosis and Treatment has cared for many families and will help you through your journey, too.

What to expect
From the moment of referral through delivery and postnatal care, your family can expect a supportive experience when you come to us with a diagnosis of a birth defect.
Resources to help
Spina bifida causes, symptoms and treatment Resources
Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment Resources
Learning your baby has a birth defect is a life-changing experience. We want you to know that you are not alone. To help you find answers to your questions, we've created this list of educational health resources.
Reviewed by N. Scott Adzick, MD, MMM, FACS, FAAP





