What is lower urinary tract obstruction (LUTO)
Lower urinary tract obstruction (LUTO) is a rare condition that occurs before birth when the urethra – the tube that connects the bladder to the amniotic fluid space around the fetus – is completely or partially blocked. LUTO occurs in around 1 in 5,000 fetuses, and is more common in males. It is also known as bladder outlet obstruction or obstructive uropathy.
In cases of complete obstruction, urine cannot be released into the amniotic space around the fetus. This causes the bladder to enlarge (megacystis) and the amniotic fluid levels around the fetus to decrease (0ligohydramnios).
Amniotic fluid is extremely important for fetal lung development. When fluid levels are low or absent, it can result in underdevelopment of the lungs (pulmonary hypoplasia), which is a life-threatening condition. The obstruction also causes the urine to back up into the kidneys, which can eventually lead to kidney damage.
In cases of partial obstruction, the bladder is enlarged; however, some amount of urine is able to escape in the amniotic cavity and the amniotic fluid around the fetus remains normal.
The most common types of blader outlet obstruction are:
- Urethral atresia (UA) — a complete obstruction of the urethra
- Posterior urethral valves (PUV) — a flap of tissue blocking the urethra
- Triad syndrome (Prune Belly syndrome) — a narrowing in the mid-portion of the urethra which highly restricts the passage of urine. It is also associated with poor development of the abdominal muscles and undescended testicles.
The prognosis for lower urinary tract obstruction varies. It depends upon the severity of the obstruction (partial vs. complete) as well as the presence or absence of additional findings.
Timely and accurate diagnosis at an experienced fetal center is essential for providing families with a complete picture of their unborn baby’s condition. It also ensures the most treatment options and best possible outcome.
What causes LUTO?
The causes of lower urinary tract obstruction are unknown, and most cases are isolated. There is an increased risk for chromosome, or in rare cases, genetic differences. For this reason, genetic testing may be recommended.
Signs and symptoms of LUTO

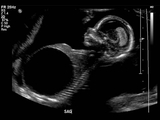
A diagnosis of LUTO is typically made during a routine prenatal ultrasound in the mid-second trimester.
The sonographer may notice:
- An enlarged and thick-walled fetal bladder
- Enlarged, echogenic kidneys and dilated ureters
- Differences in the amniotic fluid volume
In some cases, bladder enlargement is diagnosed in the first trimester of pregnancy.
Unpublished evidence suggests that approximately half of all early obstructions resolve by the end of the first trimester without long-term consequences.
Prenatal imaging and testing
A prenatal ultrasound that suggests lower urinary tract obstruction should be further evaluated at a fetal center familiar with management of these cases. More than 3,180 pregnancies with genitourinary defects like LUTO have been referred to the Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment (CFDT) at Children’s Hospital of Philadelphia (CHOP). This experience means our team sees this condition often and is prepared to provide the most expert diagnosis, management options and treatment planning.
If you choose an evaluation at our center, a knowledgeable fetal therapy coordinator will review your records, answer your questions, and arrange for a one-day comprehensive evaluation.
Our team of dedicated imaging specialists uses the most advanced prenatal imaging techniques and state of the art technologies available to gather additional details about the diagnosis. Tests will include:
- High-resolution level II ultrasound — noninvasive imaging used to assess overall fetal growth and development, severity of the obstruction, condition of the kidneys and levels of amniotic fluid volume.
- Fetal echocardiogram — a specialized ultrasound evaluation of the fetal heart to assess cardiac structure and function.
After thorough review of these tests and additional counseling, the following may be offered if indicated:
- Serial renal function (electrolyte) profile — ultrasound guided complete fetal bladder drainage (vesicocentesis) typically performed two to three times at 24-to-48-hour time intervals. Results are used to evaluate kidney function to guide further management.
- Fetal karyotype/microarray — laboratory studies using fetal urine or amniotic fluid to confirm gender and rule out abnormalities that affect survival or long-term outcome.
In rare cases, an ultrafast fetal MRI may be indicated. This is a noninvasive imaging technique pioneered at CHOP that can provide additional detail about the genitourinary tract in complex cases of bladder obstruction.
A thorough prenatal evaluation will determine whether your fetus may benefit from prenatal intervention and provide you with the information necessary to make informed decisions.
The presence of cysts in the fetal kidneys (renal dysplasia) is an indicator of irreversible kidney damage and an exclusion for shunt placement. An enlarged fetal bladder in the presence of normal amniotic fluid volume indicates a partial obstruction. These cases are typically followed by ultrasound for changes in amniotic fluid volume without prenatal intervention.
Multidisciplinary consultation
Once your initial evaluation is complete, our multidisciplinary team, led by a maternal-fetal medicine specialist, meets with you and your family to review test results, discuss the diagnosis, explain treatment options and outcomes, and answer questions.
Additional team members, including a pediatric urologist and pediatric nephrologist can provide further insight about medical and surgical needs and long-term outcomes.
To learn more about the diagnosis and treatment of LUTO, watch our video below and follow one family’s journey. (En Español »)
Prenatal intervention: Vesicoamniotic shunt and RAFT
Male fetuses with low amniotic fluid (oligohydramnios) and isolated complete obstruction without evidence of irreversible kidney damage may be candidates for fetal intervention. The standard prenatal treatment is vesicoamniotic shunt placement.
A shunt is a hollow tube that temporarily bypasses the lower urinary tract obstruction. It provides an alternate passageway for urine to flow from the bladder through the abdominal wall to the amniotic fluid space around the fetus. This allows for drainage of the urinary tract and bladder and establishes fluid around the fetus to help lung development.
The procedure is performed in the operating room (OR) under ultrasound guidance and maternal intravenous (IV) sedation. Prior to shunt placement, an amnioinfusion may be necessary in the OR. This means fluid is added to the space around the fetus to allow for shunt placement. Families typically stay close to the hospital for one week post-surgery.
Our social workers and fetal therapy coordinators are available to help coordinate housing options based upon your family’s needs.
Renal Anhydramnios Fetal Therapy (RAFT)
If a fetus has bladder outlet obstruction, kidney damage and absent amniotic fluid (anhydramnios) by 22 weeks, they may be candidates for serial amnioinfusion (amniotic fluid replacement) or expectant management under the Renal Anhydramnios Fetal Therapy (RAFT) study. The RAFT study is a National Institutes of Health (NIH)-approved multicenter clinical trial. To learn about the trial, please contact us at 215-590-5190 or visit clinical trials.gov.
Pregnancy management and delivery
Some families elect to return home for local care and delivery. Close fetal monitoring is important throughout the remainder of the pregnancy. We remain available to collaborate with your local team for questions and concerns. We can also help connect you with a local pediatric nephrologist and urologist who will be able to evaluate and treat your child after birth.
Mothers who elect to be cared for in CHOP’s Wood Center for Fetal Diagnosis and Treatment will deliver in the Garbose Family Special Delivery Unit (SDU), the world’s first birth facility designed exclusively for pregnancies complicated by birth defects. While the SDU offers the highest level of maternal care, the Newborn Infant Intensive Care Unit (N/IICU) offers the highest levels of care for your newborn — all within the same pediatric hospital.
Neonatal care
After delivery in the SDU, a team of specialists, led by a neonatologist, will evaluate and transition your baby to the Newborn/Infant Intensive Care Unit (N//ICU). In the N/IICU, pediatric urologists and nephrologists coordinate studies of kidney and bladder function and discuss what to expect in both the short- and long-term.
Surgical postnatal treatment options depend on the type of obstruction. For posterior urethral valves (PUV), endoscopic resection (valve ablation) is a minimally invasive technique performed within the first several days of life.
In other cases, a vesicostomy — an opening below the belly button that allows the bladder to drain directly into a diaper — diverts urine until the baby can undergo surgery. Learn more about how PUVs are treated by CHOP's pediatric urologists.
If the baby’s kidneys are not working properly, they might need renal replacement therapy (RRT). Our teams are specialty trained to provide various forms of neonatal renal support, including Aquadex and peritoneal dialysis.
Follow-up care
Children with LUTO are more susceptible to kidney infections and kidney failure. Some will require dialysis and a kidney transplant. Some may also experience long-term respiratory symptoms, including asthma, reactive airway disease and upper respiratory infections, as well as bladder dysfunction, poor growth and musculoskeletal concerns.
Long-term follow-up is overseen by the pediatric urologist and nephrologist, with clinic visits typically every three months for the first year of life and regularly thereafter.
Watch the following video to follow one family's LUTO diagnosis and treatment journey. En Español »

Tour our Fetal Center
The Wood Center for Fetal Diagnosis and Treatment has cared for many families and will help you through your journey, too.

What to expect
From the moment of referral through delivery and postnatal care, your family can expect a supportive experience when you come to us with a diagnosis of a birth defect.
Resources to help
Lower Urinary Tract Obstruction (LUTO) Resources
Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment Resources
Learning your baby has a birth defect is a life-changing experience. We want you to know that you are not alone. To help you find answers to your questions, we've created this list of educational health resources.








