
Philadelphia, PA – Researchers at Children’s Hospital of Philadelphia (CHOP) and the Perelman School of Medicine at the University of Pennsylvania revealed the most extensive single cell atlas of the human kidney, capturing the complexity of healthy and diseased kidneys at an unprecedented level and predicting chronic kidney disease (CKD) progression earlier in its course. The findings were published today in the journal Nature Genetics.
CKD affects more than 1 in 7 U.S. adults – an estimated 37 million Americans, according to the National Institutes of Health (NIH). The risk is even higher for Americans with diabetes or high blood pressure – the two most common causes of CKD.

“CKD is rare in children, but for those affected, it can be a very serious life-altering condition,” said Jonathan Levisohn,” MD, PhD, one of the first authors and a pediatric nephrology fellow in the Division of Nephrology at CHOP. “It is also clear that while CKD most commonly affects older individuals, the risk for developing the disease starts to accrue much earlier, starting during gestation and childhood.”
Senior study author Katalin Susztak, MD, PhD, emphasized that the findings fill a critical knowledge gap by presenting the first ever roadmap of the human kidneys that includes the analysis of spatial relationship of the cells.
“Human kidneys are intricate three-dimensional structures in the body, but until this research, the spatial and molecular principles of kidney health and disease were not well understood,” said Susztak, Co-Leader of the Penn-CHOP Kidney Innovation Center, a research collaboration between CHOP and Penn-Medicine focused on transforming patient care through early detection, prevention and treatment of kidney disease and its complications across the lifespan. “We now have a powerful tool for prognosis, outperforming traditional histopathological analysis especially in early-stage kidney disease.”

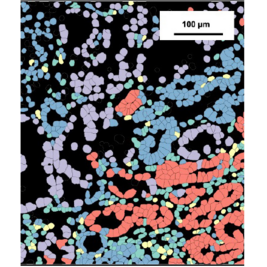
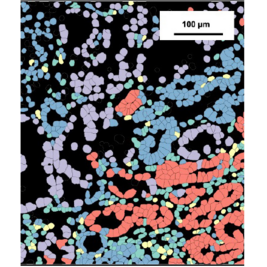
In the study, Susztak and her team analyzed more than 700,000 cells from 81 kidney samples in patients from ages 24 to 90. The researchers used machine learning to develop the high-resolution atlas, allowing them to integrate multi-omics data, map cellular and spatial information, identify tissue microenvironments and develop predictive models for kidney disease progression.
Key findings include identification of 44 main and 114 distinct cell sub-types or states in both healthy and CKD-affected human kidneys. The researchers identified four distinct spatial microenvironments based on gene expression: glomerular, immune, tubule and fibrotic.
Fibrosis is a common manifestation across all forms of progressive CKD with most prior studies focusing on its predictive ability in severe cases. Glomerular filtration rate (GFR) and albuminuria predict kidney function decline reasonably well in advanced CKD, but prognosis is challenging in earlier disease stages. In this study, however, data revealed a gene signature in the fibrotic microenvironment (FME-GS), that can classify kidney samples and predict future kidney function decline.
The team plans to further define the fibrotic microenvironment, validate its predictive power in additional cohorts and understand the underlying mechanisms. They aim to explore therapeutic targets within the fibrotic microenvironment, potentially paving the way for new treatments to halt or reverse kidney fibrosis.
“Although foundational, we envision the clinical implications of this study to be potentially profound, as this new understanding can lead to better diagnostics and precision treatments for patients with chronic kidney disease,” said Susztak, who is also a Professor of Medicine at Penn.
Work in the Susztak Lab is supported by the National Institutes of Health grants P50DK114786, DK076077, DK087635, DK132630 and DK105821. The study is also supported by GSK, Regeneron, Boehringer Ingelheim and Novo Nordisk. The funders have no influence on the reported results. Additional support for this work was provided by the Ben Lipps Fellowship. the Deutsche Forschungsgemeinschaft German Research Foundation grant DU 2449/1-1, the MOLMED Ph.D. program at the Medical University of Graz, a Marietta-Blau Grant and an Austrian Marshall Plan Foundation scholarship.

Abedini and Levinsohn et al. “Single-cell multi-omic and spatial profiling of human kidneys implicates the fibrotic microenvironment in kidney disease progression.” July 24th, 2024. Nature Genetics. DOI: 10.1038/s41588-024-01802-x
About Children’s Hospital of Philadelphia:
A non-profit, charitable organization, Children’s Hospital of Philadelphia was founded in 1855 as the nation’s first pediatric hospital. Through its long-standing commitment to providing exceptional patient care, training new generations of pediatric healthcare professionals, and pioneering major research initiatives, the hospital has fostered many discoveries that have benefited children worldwide. Its pediatric research program is among the largest in the country. The institution has a well-established history of providing advanced pediatric care close to home through its CHOP Care Network, which includes more than 50 primary care practices, specialty care and surgical centers, urgent care centers, and community hospital alliances throughout Pennsylvania and New Jersey, as well as the Middleman Family Pavilion and its dedicated pediatric emergency department in King of Prussia. In addition, its unique family-centered care and public service programs have brought Children’s Hospital of Philadelphia recognition as a leading advocate for children and adolescents. For more information, visit https://www.chop.edu.
Philadelphia, PA – Researchers at Children’s Hospital of Philadelphia (CHOP) and the Perelman School of Medicine at the University of Pennsylvania revealed the most extensive single cell atlas of the human kidney, capturing the complexity of healthy and diseased kidneys at an unprecedented level and predicting chronic kidney disease (CKD) progression earlier in its course. The findings were published today in the journal Nature Genetics.
CKD affects more than 1 in 7 U.S. adults – an estimated 37 million Americans, according to the National Institutes of Health (NIH). The risk is even higher for Americans with diabetes or high blood pressure – the two most common causes of CKD.

“CKD is rare in children, but for those affected, it can be a very serious life-altering condition,” said Jonathan Levisohn,” MD, PhD, one of the first authors and a pediatric nephrology fellow in the Division of Nephrology at CHOP. “It is also clear that while CKD most commonly affects older individuals, the risk for developing the disease starts to accrue much earlier, starting during gestation and childhood.”
Senior study author Katalin Susztak, MD, PhD, emphasized that the findings fill a critical knowledge gap by presenting the first ever roadmap of the human kidneys that includes the analysis of spatial relationship of the cells.
“Human kidneys are intricate three-dimensional structures in the body, but until this research, the spatial and molecular principles of kidney health and disease were not well understood,” said Susztak, Co-Leader of the Penn-CHOP Kidney Innovation Center, a research collaboration between CHOP and Penn-Medicine focused on transforming patient care through early detection, prevention and treatment of kidney disease and its complications across the lifespan. “We now have a powerful tool for prognosis, outperforming traditional histopathological analysis especially in early-stage kidney disease.”

In the study, Susztak and her team analyzed more than 700,000 cells from 81 kidney samples in patients from ages 24 to 90. The researchers used machine learning to develop the high-resolution atlas, allowing them to integrate multi-omics data, map cellular and spatial information, identify tissue microenvironments and develop predictive models for kidney disease progression.
Key findings include identification of 44 main and 114 distinct cell sub-types or states in both healthy and CKD-affected human kidneys. The researchers identified four distinct spatial microenvironments based on gene expression: glomerular, immune, tubule and fibrotic.
Fibrosis is a common manifestation across all forms of progressive CKD with most prior studies focusing on its predictive ability in severe cases. Glomerular filtration rate (GFR) and albuminuria predict kidney function decline reasonably well in advanced CKD, but prognosis is challenging in earlier disease stages. In this study, however, data revealed a gene signature in the fibrotic microenvironment (FME-GS), that can classify kidney samples and predict future kidney function decline.
The team plans to further define the fibrotic microenvironment, validate its predictive power in additional cohorts and understand the underlying mechanisms. They aim to explore therapeutic targets within the fibrotic microenvironment, potentially paving the way for new treatments to halt or reverse kidney fibrosis.
“Although foundational, we envision the clinical implications of this study to be potentially profound, as this new understanding can lead to better diagnostics and precision treatments for patients with chronic kidney disease,” said Susztak, who is also a Professor of Medicine at Penn.
Work in the Susztak Lab is supported by the National Institutes of Health grants P50DK114786, DK076077, DK087635, DK132630 and DK105821. The study is also supported by GSK, Regeneron, Boehringer Ingelheim and Novo Nordisk. The funders have no influence on the reported results. Additional support for this work was provided by the Ben Lipps Fellowship. the Deutsche Forschungsgemeinschaft German Research Foundation grant DU 2449/1-1, the MOLMED Ph.D. program at the Medical University of Graz, a Marietta-Blau Grant and an Austrian Marshall Plan Foundation scholarship.

Abedini and Levinsohn et al. “Single-cell multi-omic and spatial profiling of human kidneys implicates the fibrotic microenvironment in kidney disease progression.” July 24th, 2024. Nature Genetics. DOI: 10.1038/s41588-024-01802-x
About Children’s Hospital of Philadelphia:
A non-profit, charitable organization, Children’s Hospital of Philadelphia was founded in 1855 as the nation’s first pediatric hospital. Through its long-standing commitment to providing exceptional patient care, training new generations of pediatric healthcare professionals, and pioneering major research initiatives, the hospital has fostered many discoveries that have benefited children worldwide. Its pediatric research program is among the largest in the country. The institution has a well-established history of providing advanced pediatric care close to home through its CHOP Care Network, which includes more than 50 primary care practices, specialty care and surgical centers, urgent care centers, and community hospital alliances throughout Pennsylvania and New Jersey, as well as the Middleman Family Pavilion and its dedicated pediatric emergency department in King of Prussia. In addition, its unique family-centered care and public service programs have brought Children’s Hospital of Philadelphia recognition as a leading advocate for children and adolescents. For more information, visit https://www.chop.edu.
Contact us
Jennifer Lee