Adam Kronish, MD, and Krishna White, MD, MPH
As the school year gets underway, the adolescent annual visits, pre-participation sports evaluations, and driving forms fill pediatrician offices. These critical touchpoints with the healthcare system provide opportunities for pediatricians to discuss and prevent lifetime illnesses that emerge in adolescence and young adulthood. Mental health disorders fall under this category, and substance use disorders (SUDs) are mental health disorders.
Pediatricians possess the skills to screen, briefly intervene, and refer to addiction treatment (SBIRT) as recommended by the American Academy of Pediatrics (AAP), yet significant gaps in the implementation of the SBIRT framework have been identified. Primary care pediatricians can bridge the gap in initiating treatment for SUDs in adolescents and young adults (AYAs) by building on current practices in screening, gathering a thorough social history, and integrating mental health into pediatric primary care practices.
Validated screening tools for SUDs in AYAs exist, including the 7-item Screening to Brief Intervention (S2BI) and 9-item CRAFFT questionnaires, which are easily incorporated into intake forms and are utilized at Children’s Hospital of Philadelphia (CHOP) primary care sites as part of the Adolescent Health Questionnaire (AHQ).
PCP’s Response to a Positive Screen
If a patient screens positive, providers who care for young people can assess the level of substance use the patient is engaging in: experimental, daily, problematic use, or having a substance use disorder. Although the DSM-V has explicit criteria for SUD, the distinguishing factor for the disorder is that the patterns of behavior impair daily functioning. For SUDs, this manifests as the 3 Cs: cravings, lack of control, and continued use despite negative consequences. If these are occurring, an AYA may benefit from treatment of SUD with behavioral and medication intervention.
Any pediatrician can prescribe medications for substance use disorders. In adolescents, medications have been studied for nicotine, alcohol, and opioid use disorders.
- For nicotine use disorder, nicotine replacement therapy, bupropion, and varenicline have been studied in adolescents.
- For alcohol use disorder, oral naltrexone (at a starting dose of 25 mg and up to the standard adult dose of 50 mg daily) can be safely used in adolescents without concurrent opioid use.
- For opioid use disorder, the AAP offers online trainings to teach pediatricians how to manage medications for opioid use disorder: buprenorphine and naltrexone
Pediatricians who are uncomfortable managing SUDs can refer to an adolescent, addiction medicine, or psychiatric specialist who focuses on this area.
Keeping Patients Safe
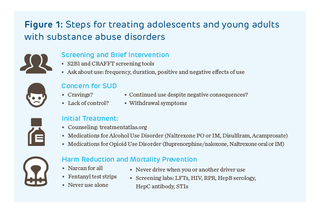
One final aspect of approaching adolescents with substance use disorders derives from empathy and individualization of care: keeping patients safe using harm reduction and overdose prevention. Although our instinct as pediatricians is to promote abstinence, this does not always align with a young person’s goals or stage of change at a point in time. In that case, pediatricians can continue to partner with young people and their families to use strategies that minimize the risk of injury, disease, or death related to continued substance use.
Examples are listed in Figure 1 and include expanded access to naloxone (now available over the counter), using fentanyl test strips, and screening for behavioral and infectious comorbidities of substance use.
When the mental health needs of young people have exceeded the number of mental health providers, pediatricians have stepped up to fill that role. Pediatricians have incorporated the medication management of depression, anxiety, and ADHD into general practice; a similar model can be applied to SUDs with support and expert consultation for complex cases.
References and Suggested Readings
Levy SJ, Williams JF; Committee on Substance Use and Prevention. Substance use screening, brief intervention, and referral to treatment. Pediatrics. 2016;138(1):e20161211.
Calihan JB, Levy S. Substance use screening, brief intervention, and referral to treatment in pediatric primary care, school-based health clinics, and mental health clinics. Psychiatr Clin North Am. 2023;46(4):749-760.
Levy S, Weitzman ER, Marin AC, et al. Sensitivity and specificity of S2BI for identifying alcohol and cannabis use disorders among adolescents presenting for primary care. Subst Abus. 2021;42(3):388-395.
Kulak JA, Griswold KS. Adolescent substance use and misuse: recognition and management. Am Fam Physician. 2019;99(11):689-696.
Substance Abuse and Mental Health Services Administration. Waiver Elimination for MAT Act. https://www.samhsa.gov/medications-substance- use-disorders/waiver-elimination-mat-act. Accessed September 4, 2024.
Jenssen BP, DiFiore G, Powell M, et al. Accelerating innovation in primary care to support adolescent health discussions. Pediatrics. 2024;154(1):e2023064285.
Malhotra A, Drexler K, Hsu M, Tang YL. Medication treatment for alcohol use disorder in special populations. Am J Addict. 2023;32(5):433-441.
American Academy of Pediatrics. Patient Care Website. Training to treat opioid use disorder in adolescents. https://www.aap.org/en/patient-care/substance-use-and-prevention/?srsltid=AfmBOopFCMnhf9btMtgRLsB247gJcKuqBWTHtLI0FQ1axMrHS1GhRRdE Accessed September 4, 2024
Featured in this article
Experts
Adam Kronish, MD, and Krishna White, MD, MPH
As the school year gets underway, the adolescent annual visits, pre-participation sports evaluations, and driving forms fill pediatrician offices. These critical touchpoints with the healthcare system provide opportunities for pediatricians to discuss and prevent lifetime illnesses that emerge in adolescence and young adulthood. Mental health disorders fall under this category, and substance use disorders (SUDs) are mental health disorders.
Pediatricians possess the skills to screen, briefly intervene, and refer to addiction treatment (SBIRT) as recommended by the American Academy of Pediatrics (AAP), yet significant gaps in the implementation of the SBIRT framework have been identified. Primary care pediatricians can bridge the gap in initiating treatment for SUDs in adolescents and young adults (AYAs) by building on current practices in screening, gathering a thorough social history, and integrating mental health into pediatric primary care practices.
Validated screening tools for SUDs in AYAs exist, including the 7-item Screening to Brief Intervention (S2BI) and 9-item CRAFFT questionnaires, which are easily incorporated into intake forms and are utilized at Children’s Hospital of Philadelphia (CHOP) primary care sites as part of the Adolescent Health Questionnaire (AHQ).
PCP’s Response to a Positive Screen
If a patient screens positive, providers who care for young people can assess the level of substance use the patient is engaging in: experimental, daily, problematic use, or having a substance use disorder. Although the DSM-V has explicit criteria for SUD, the distinguishing factor for the disorder is that the patterns of behavior impair daily functioning. For SUDs, this manifests as the 3 Cs: cravings, lack of control, and continued use despite negative consequences. If these are occurring, an AYA may benefit from treatment of SUD with behavioral and medication intervention.
Any pediatrician can prescribe medications for substance use disorders. In adolescents, medications have been studied for nicotine, alcohol, and opioid use disorders.
- For nicotine use disorder, nicotine replacement therapy, bupropion, and varenicline have been studied in adolescents.
- For alcohol use disorder, oral naltrexone (at a starting dose of 25 mg and up to the standard adult dose of 50 mg daily) can be safely used in adolescents without concurrent opioid use.
- For opioid use disorder, the AAP offers online trainings to teach pediatricians how to manage medications for opioid use disorder: buprenorphine and naltrexone
Pediatricians who are uncomfortable managing SUDs can refer to an adolescent, addiction medicine, or psychiatric specialist who focuses on this area.
Keeping Patients Safe
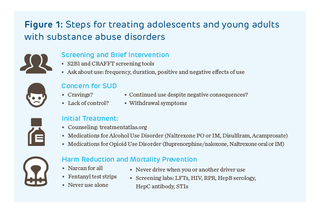
One final aspect of approaching adolescents with substance use disorders derives from empathy and individualization of care: keeping patients safe using harm reduction and overdose prevention. Although our instinct as pediatricians is to promote abstinence, this does not always align with a young person’s goals or stage of change at a point in time. In that case, pediatricians can continue to partner with young people and their families to use strategies that minimize the risk of injury, disease, or death related to continued substance use.
Examples are listed in Figure 1 and include expanded access to naloxone (now available over the counter), using fentanyl test strips, and screening for behavioral and infectious comorbidities of substance use.
When the mental health needs of young people have exceeded the number of mental health providers, pediatricians have stepped up to fill that role. Pediatricians have incorporated the medication management of depression, anxiety, and ADHD into general practice; a similar model can be applied to SUDs with support and expert consultation for complex cases.
References and Suggested Readings
Levy SJ, Williams JF; Committee on Substance Use and Prevention. Substance use screening, brief intervention, and referral to treatment. Pediatrics. 2016;138(1):e20161211.
Calihan JB, Levy S. Substance use screening, brief intervention, and referral to treatment in pediatric primary care, school-based health clinics, and mental health clinics. Psychiatr Clin North Am. 2023;46(4):749-760.
Levy S, Weitzman ER, Marin AC, et al. Sensitivity and specificity of S2BI for identifying alcohol and cannabis use disorders among adolescents presenting for primary care. Subst Abus. 2021;42(3):388-395.
Kulak JA, Griswold KS. Adolescent substance use and misuse: recognition and management. Am Fam Physician. 2019;99(11):689-696.
Substance Abuse and Mental Health Services Administration. Waiver Elimination for MAT Act. https://www.samhsa.gov/medications-substance- use-disorders/waiver-elimination-mat-act. Accessed September 4, 2024.
Jenssen BP, DiFiore G, Powell M, et al. Accelerating innovation in primary care to support adolescent health discussions. Pediatrics. 2024;154(1):e2023064285.
Malhotra A, Drexler K, Hsu M, Tang YL. Medication treatment for alcohol use disorder in special populations. Am J Addict. 2023;32(5):433-441.
American Academy of Pediatrics. Patient Care Website. Training to treat opioid use disorder in adolescents. https://www.aap.org/en/patient-care/substance-use-and-prevention/?srsltid=AfmBOopFCMnhf9btMtgRLsB247gJcKuqBWTHtLI0FQ1axMrHS1GhRRdE Accessed September 4, 2024