Case:
Avery, a 5-year-old male, presents to the pediatrician for his well-child visit. His parents report that he is growing and developing well, but that they are concerned about recurrent nosebleeds that are happening most nights over the past week.
He has previously had intermittent episodes of epistaxis, and they tend to occur at night resulting in “a lot” of blood all over the pillow and sheets. He tends to get the nosebleeds for several nights in a row and may also get daytime nosebleeds during these periods of bleeding. The nosebleeds can last for 20 to 30 minutes before they are stopped. The family has been pinching the nose for 5-minute intervals to stop the nosebleeds.
He also has a history of easy bruising and recently started playing soccer and they have noted bumps on his shins under the bruises.
The family has previously reported concerns about bleeding, and screening studies have shown a normal CBC (platelet count 203k/mcL), normal PT (11.3s) and normal PTT (29.6s) and normal vonWillebrand Factor (vWF) screening tests (vWF antigen: 98%; vwF activity: 103%; F8 activity: 115%).
Platelet Storage Pool Deficiency (SPD)
Discussion:
Platelet function disorders are an underrecognized group of bleeding disorders that can present with variable bleeding starting childhood. While epistaxis and bruising are common complaints to the pediatrician, bruising with a palpable component should raise suspicion for a bleeding disorder, as should epistaxis that is prolonged (although this may also be a sign that families have not been following proper advice on epistaxis management).
Platelet function disorders are a heterogeneous group of disorders and may present with mild bleeding symptoms without coagulation abnormalities as described in the case above. Platelet count may be normal, but bleeding results because the platelets are not able to perform their functions normally—either because of surface receptor problems, signaling problems internally within the platelet, or problems with granules or granule contents. The most common non-syndromic platelet function disorder is the platelet storage pool deficiency (SPD), which probably encompasses many pathophysiologic and molecular causes that result in the same clinical outcomes.
Platelets contain two major types of granules necessary for optimal function: alpha granules and delta (dense) granules (see Figure 1a). In the platelet SPDs, platelets are missing either alpha granules (which make platelets purple under the microscope by Wright-Geimsa stain) or delta granules (dense granules because they are dark dots by electron microscopy due to their calcium content when platelets are whole mounted for this study). Platelets that lack alpha granules are characteristically “grey” on microscopy resulting in the “grey platelet syndrome” (see Figure 1b, compared to normal in c), but other SPDs may have a decrease in alpha granules, absence or decrease in dense granules, or a mix of both.
Specialized Testing Needed for Diagnosis
Diagnosis of SPD requires referral to a hematologist, who will need to arrange for both platelet function testing and evaluation of platelet morphology by electron microscopy. Molecular testing may also be required.
Although they are the most common type of platelet disorder, the molecular biology of SPD is still poorly understood. So far, only grey platelet syndrome has had the molecular biology clearly defined, perhaps because the phenotype is so much clearer than the other platelet SPDs. A few different genes have been associated with dense granule deficiencies, but most of those disorders are associated with other, syndromic features, such as albinism, or other granule problems within the immune system or nervous system.
This patient was referred to hematology and platelet function studies demonstrated abnormal platelet function with abnormal aggregation and secretion with ADP and epinephrine with an absent secondary aggregation wave with epinephrine—a classic finding in SPD. Platelet electron microscopy demonstrated absent dense granules (see Figure 1e, compared to normal in d).
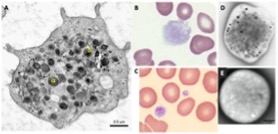
Figure 1:
A. Platelet by transmission electron microscopy showing alpha granules (a), delta granules (s). Platelet image courtesy of TEM by University of New South Wales.
B. Grey platelets by Geimsa stain. Image courtesy of American Society of Hematology Image bank.
C. Normal platelet by Geimsa stain.
D. Normal platelet by whole mount electron microscopy with dense granules (arrows). J. Clin. Med. 2020;9(6):1734.
E. Dense granule deficiency by electron microscopy. J. Clin. Med. 2020:9(8):2508.
Mild Bleeding Outside of Trauma, Surgery, Pregnancy
In general, bleeding with SPD is mild, although bleeding can be increased with surgery and trauma, especially dental trauma or surgery. Women with SPD can have abnormal uterine bleeding or bleeding with pregnancy and delivery. Girls can have hemorrhage with menarche.
For these reasons, making the diagnosis is important, so counseling can be provided about when to seek care and what information to provide other healthcare workers. Medications that inhibit platelet function ,such as aspirin and non-steroidal anti-inflammatory medications, should be avoided as they may increase bleeding symptoms.
Anti-fibrinolytic therapies such as aminocaproic acid or tranexamic acid can be very helpful to decrease mucosal bleeding symptoms and hormonal therapy is the best option for abnormal uterine bleeding. Platelet transfusions may be needed for significant bleeding but are rarely routinely required. Families are counseled that the child should avoid activities with high risk of trauma or bleeding, and this includes avoiding high-risk contact sports such as ice hockey, boxing and football.
The Division of Hematology at CHOP now has a Pediatric Platelet Disorder Program with dedicated physician, nursing, social work, genetic counseling, and behavioral health staff dedicated to supporting our families with new and established diagnoses of platelet disorders and approaching these patients with a wholistic, family-centric view.
When to Refer for Suspected Platelet Disorder:
- Palpable bruises without history of trauma
- Prolonged surgical- or trauma-related bleeding
- Family history of abnormal bleeding or platelet disorder
- Abnormal uterine bleeding with onset at menarche (in collaboration with adolescent health)
- Recurrent petechial rash
- Other unexplained mucosal bleeding (GI, GU or mouth/gums)
Case:
Avery, a 5-year-old male, presents to the pediatrician for his well-child visit. His parents report that he is growing and developing well, but that they are concerned about recurrent nosebleeds that are happening most nights over the past week.
He has previously had intermittent episodes of epistaxis, and they tend to occur at night resulting in “a lot” of blood all over the pillow and sheets. He tends to get the nosebleeds for several nights in a row and may also get daytime nosebleeds during these periods of bleeding. The nosebleeds can last for 20 to 30 minutes before they are stopped. The family has been pinching the nose for 5-minute intervals to stop the nosebleeds.
He also has a history of easy bruising and recently started playing soccer and they have noted bumps on his shins under the bruises.
The family has previously reported concerns about bleeding, and screening studies have shown a normal CBC (platelet count 203k/mcL), normal PT (11.3s) and normal PTT (29.6s) and normal vonWillebrand Factor (vWF) screening tests (vWF antigen: 98%; vwF activity: 103%; F8 activity: 115%).
Platelet Storage Pool Deficiency (SPD)
Discussion:
Platelet function disorders are an underrecognized group of bleeding disorders that can present with variable bleeding starting childhood. While epistaxis and bruising are common complaints to the pediatrician, bruising with a palpable component should raise suspicion for a bleeding disorder, as should epistaxis that is prolonged (although this may also be a sign that families have not been following proper advice on epistaxis management).
Platelet function disorders are a heterogeneous group of disorders and may present with mild bleeding symptoms without coagulation abnormalities as described in the case above. Platelet count may be normal, but bleeding results because the platelets are not able to perform their functions normally—either because of surface receptor problems, signaling problems internally within the platelet, or problems with granules or granule contents. The most common non-syndromic platelet function disorder is the platelet storage pool deficiency (SPD), which probably encompasses many pathophysiologic and molecular causes that result in the same clinical outcomes.
Platelets contain two major types of granules necessary for optimal function: alpha granules and delta (dense) granules (see Figure 1a). In the platelet SPDs, platelets are missing either alpha granules (which make platelets purple under the microscope by Wright-Geimsa stain) or delta granules (dense granules because they are dark dots by electron microscopy due to their calcium content when platelets are whole mounted for this study). Platelets that lack alpha granules are characteristically “grey” on microscopy resulting in the “grey platelet syndrome” (see Figure 1b, compared to normal in c), but other SPDs may have a decrease in alpha granules, absence or decrease in dense granules, or a mix of both.
Specialized Testing Needed for Diagnosis
Diagnosis of SPD requires referral to a hematologist, who will need to arrange for both platelet function testing and evaluation of platelet morphology by electron microscopy. Molecular testing may also be required.
Although they are the most common type of platelet disorder, the molecular biology of SPD is still poorly understood. So far, only grey platelet syndrome has had the molecular biology clearly defined, perhaps because the phenotype is so much clearer than the other platelet SPDs. A few different genes have been associated with dense granule deficiencies, but most of those disorders are associated with other, syndromic features, such as albinism, or other granule problems within the immune system or nervous system.
This patient was referred to hematology and platelet function studies demonstrated abnormal platelet function with abnormal aggregation and secretion with ADP and epinephrine with an absent secondary aggregation wave with epinephrine—a classic finding in SPD. Platelet electron microscopy demonstrated absent dense granules (see Figure 1e, compared to normal in d).
Figure 1:
A. Platelet by transmission electron microscopy showing alpha granules (a), delta granules (s). Platelet image courtesy of TEM by University of New South Wales.
B. Grey platelets by Geimsa stain. Image courtesy of American Society of Hematology Image bank.
C. Normal platelet by Geimsa stain.
D. Normal platelet by whole mount electron microscopy with dense granules (arrows). J. Clin. Med. 2020;9(6):1734.
E. Dense granule deficiency by electron microscopy. J. Clin. Med. 2020:9(8):2508.
Mild Bleeding Outside of Trauma, Surgery, Pregnancy
In general, bleeding with SPD is mild, although bleeding can be increased with surgery and trauma, especially dental trauma or surgery. Women with SPD can have abnormal uterine bleeding or bleeding with pregnancy and delivery. Girls can have hemorrhage with menarche.
For these reasons, making the diagnosis is important, so counseling can be provided about when to seek care and what information to provide other healthcare workers. Medications that inhibit platelet function ,such as aspirin and non-steroidal anti-inflammatory medications, should be avoided as they may increase bleeding symptoms.
Anti-fibrinolytic therapies such as aminocaproic acid or tranexamic acid can be very helpful to decrease mucosal bleeding symptoms and hormonal therapy is the best option for abnormal uterine bleeding. Platelet transfusions may be needed for significant bleeding but are rarely routinely required. Families are counseled that the child should avoid activities with high risk of trauma or bleeding, and this includes avoiding high-risk contact sports such as ice hockey, boxing and football.
The Division of Hematology at CHOP now has a Pediatric Platelet Disorder Program with dedicated physician, nursing, social work, genetic counseling, and behavioral health staff dedicated to supporting our families with new and established diagnoses of platelet disorders and approaching these patients with a wholistic, family-centric view.
When to Refer for Suspected Platelet Disorder:
- Palpable bruises without history of trauma
- Prolonged surgical- or trauma-related bleeding
- Family history of abnormal bleeding or platelet disorder
- Abnormal uterine bleeding with onset at menarche (in collaboration with adolescent health)
- Recurrent petechial rash
- Other unexplained mucosal bleeding (GI, GU or mouth/gums)