Case: An 11-year-old girl with no significant past medical or surgical history presented to her PCP after approximately 2 months of progressive hoarseness and exertional stridor and dyspnea. During this time, she had begun to cough up thick mucus that felt like it was stuck in her throat, but she had not had any recent illness or viral infection. In addition to difficulty breathing, she had reported “throwing up in her mouth” every day and experiencing pain with swallowing. She had no history of choking or coughing with eating and drinking.
She had never passed out due to shortness of breath, but she was no longer able to complete in soccer at the level she had previously enjoyed. She was playing for only brief stints and then had to come out to rest. Her PCP diagnosed her with asthma and started her on albuterol and QVAR 40 to be used on an as needed basis. When inhalers did not help, she was referred to Pulmonology where pulmonary function testing revealed limited flow on both inspiratory and expiratory flow volume curves. ENT evaluation was noteworthy for mild biphasic stridor but non-labored breathing. Nasopharyngoscopy was unremarkable with normal vocal fold movement bilaterally.
Discussion: Following urgent bronchoscopy and extensive subsequent evaluation with CHOP’s Center for Pediatric Airway Disorders and CHOP Rheumatology, this patient was ultimately diagnosed with idiopathic subglottic/tracheal stenosis (iSGS), a rare cause of airway narrowing in children.
In developing a differential diagnosis for a pediatric patient with exertional dyspnea, cough, stridor, or dysphonia, it is important to first consider other more common etiologies, including vocal cord dysfunction (VCD), asthma, eosinophilic esophagitis (EoE), or even respiratory papillomatosis. However, the progressive nature of her symptoms coupled with the biphasic stridor and flow volume curves hinted at something more significant.
Idiopathic SGS has an annual incidence of 1:400,000. Impacted patients are almost exclusively women, predominantly middle-aged (mean 50 years), and usually Caucasian. The incidence in the pediatric population, though, is far less with only a few case reports described in the literature. As the name implies, the pathophysiology is not well understood, though it has been postulated that hormonal changes, reflux, or even specific bacterium within the airway microbiome may play a role in its evolution.
Overlapping symptoms often delay diagnosis
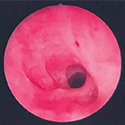
It is far more common to encounter acquired subglottic or tracheal stenosis following a history of prolonged intubation for mechanical ventilation, airway trauma, infection, or vasculitis, such as granulomatosis with polyangiitis (GPA). Idiopathic subglottic stenosis is a fibroinflammatory disease process that impacts the upper trachea and subglottic airway resulting in circumferential narrowing of the airway leading to dyspnea, stridor, hoarseness, and cough as common presenting symptoms. The insidious nature of its presentation and overlap with several other far more common conditions frequently leads to a delay in the diagnosis of iSGS. Patients often adapt to their progressively narrowing airway so that by the time they are diagnosed, the degree of narrowing can be significant.
The CHOP Center for Pediatric Airway Disorders offers patients like this the opportunity to be seen and evaluated by a multidisciplinary team of ENT, GI, and Pulmonary physicians and nurse practitioners, as well as speech and language pathologists. Evaluation in the Airway Clinic usually involves a flexible laryngoscopic evaluation of the vocal folds and upper airway. In children, visualization of the subglottis and trachea may be challenging in the outpatient clinic, so formal airway evaluation under anesthesia is often recommended. In addition to microlaryngoscopy and bronchoscopy for potential intervention, a triple endoscopy, including esophagogastroduodenoscopy (EGD) and impedance probe placement as well as flexible bronchoscopy with bronchoalveolar lavage, is often performed. This thorough approach helps the center to identify and manage not only the common airway pathologies, but also many rare cases like iSGS.
Management of iSGS, patient outcome

Management of iSGS involves both endoscopic and open surgical approaches.
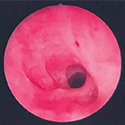
The mainstay of endoscopic management involves lysis and balloon dilation of the narrowed segment with intralesional or topical application of corticosteroids.
Unfortunately, endoscopic treatment is not curative and often has to be repeated at regular intervals as the stenosis recurs.
Surgical resection of the involved segment of airway carries greater procedural risk but can be definitive.
Following initial endoscopic management, our patient experienced near resolution of symptoms and normalization of her PFTs.
To rule out GPA and other autoimmune disorders, she was evaluated by CHOP Rheumatology and was started on azathioprine monotherapy in the hope this would offer disease- modifying adjuvant therapy.
In the years since diagnosis, she has continued to require frequent endoscopic procedures, though after the initiation of azathioprine, the interval between surgical interventions has steadily increased.

In the future, if her disease should progress or fail to respond to systemic therapy and endoscopic treatment, then surgical resection of the entire involved segment may be required.
References and suggested readings:
Gelbard A, Donovan DT, Ongkasuwan J, et al. Disease homogeneity and treatment heterogeneity in idiopathic subglottic stenosis. Laryngoscope. 2016;126(6):1390-1396.
Mark EJ, Meng F, Kradin RL, et al. Idiopathic tracheal stenosis: a clinicopathologic study of 63 cases and comparison of the pathology with chondromalacia. Am J Surg Pathol. 2008;32(8):1138-1143.
Blumin JH, Johnston N. Evidence of extraesophageal reflux in idiopathic subglottic stenosis. Laryngoscope. 2011;121(6):1266-1273.
Gelbard A, Katsantonis NG, Mizuta M, et al. Molecular analysis of idiopathic subglottic stenosis for Mycobacterium species. Laryngoscope. 2017;127(1): 179-185.
Case: An 11-year-old girl with no significant past medical or surgical history presented to her PCP after approximately 2 months of progressive hoarseness and exertional stridor and dyspnea. During this time, she had begun to cough up thick mucus that felt like it was stuck in her throat, but she had not had any recent illness or viral infection. In addition to difficulty breathing, she had reported “throwing up in her mouth” every day and experiencing pain with swallowing. She had no history of choking or coughing with eating and drinking.
She had never passed out due to shortness of breath, but she was no longer able to complete in soccer at the level she had previously enjoyed. She was playing for only brief stints and then had to come out to rest. Her PCP diagnosed her with asthma and started her on albuterol and QVAR 40 to be used on an as needed basis. When inhalers did not help, she was referred to Pulmonology where pulmonary function testing revealed limited flow on both inspiratory and expiratory flow volume curves. ENT evaluation was noteworthy for mild biphasic stridor but non-labored breathing. Nasopharyngoscopy was unremarkable with normal vocal fold movement bilaterally.
Discussion: Following urgent bronchoscopy and extensive subsequent evaluation with CHOP’s Center for Pediatric Airway Disorders and CHOP Rheumatology, this patient was ultimately diagnosed with idiopathic subglottic/tracheal stenosis (iSGS), a rare cause of airway narrowing in children.
In developing a differential diagnosis for a pediatric patient with exertional dyspnea, cough, stridor, or dysphonia, it is important to first consider other more common etiologies, including vocal cord dysfunction (VCD), asthma, eosinophilic esophagitis (EoE), or even respiratory papillomatosis. However, the progressive nature of her symptoms coupled with the biphasic stridor and flow volume curves hinted at something more significant.
Idiopathic SGS has an annual incidence of 1:400,000. Impacted patients are almost exclusively women, predominantly middle-aged (mean 50 years), and usually Caucasian. The incidence in the pediatric population, though, is far less with only a few case reports described in the literature. As the name implies, the pathophysiology is not well understood, though it has been postulated that hormonal changes, reflux, or even specific bacterium within the airway microbiome may play a role in its evolution.
Overlapping symptoms often delay diagnosis
It is far more common to encounter acquired subglottic or tracheal stenosis following a history of prolonged intubation for mechanical ventilation, airway trauma, infection, or vasculitis, such as granulomatosis with polyangiitis (GPA). Idiopathic subglottic stenosis is a fibroinflammatory disease process that impacts the upper trachea and subglottic airway resulting in circumferential narrowing of the airway leading to dyspnea, stridor, hoarseness, and cough as common presenting symptoms. The insidious nature of its presentation and overlap with several other far more common conditions frequently leads to a delay in the diagnosis of iSGS. Patients often adapt to their progressively narrowing airway so that by the time they are diagnosed, the degree of narrowing can be significant.
The CHOP Center for Pediatric Airway Disorders offers patients like this the opportunity to be seen and evaluated by a multidisciplinary team of ENT, GI, and Pulmonary physicians and nurse practitioners, as well as speech and language pathologists. Evaluation in the Airway Clinic usually involves a flexible laryngoscopic evaluation of the vocal folds and upper airway. In children, visualization of the subglottis and trachea may be challenging in the outpatient clinic, so formal airway evaluation under anesthesia is often recommended. In addition to microlaryngoscopy and bronchoscopy for potential intervention, a triple endoscopy, including esophagogastroduodenoscopy (EGD) and impedance probe placement as well as flexible bronchoscopy with bronchoalveolar lavage, is often performed. This thorough approach helps the center to identify and manage not only the common airway pathologies, but also many rare cases like iSGS.
Management of iSGS, patient outcome

Management of iSGS involves both endoscopic and open surgical approaches.
The mainstay of endoscopic management involves lysis and balloon dilation of the narrowed segment with intralesional or topical application of corticosteroids.
Unfortunately, endoscopic treatment is not curative and often has to be repeated at regular intervals as the stenosis recurs.
Surgical resection of the involved segment of airway carries greater procedural risk but can be definitive.
Following initial endoscopic management, our patient experienced near resolution of symptoms and normalization of her PFTs.
To rule out GPA and other autoimmune disorders, she was evaluated by CHOP Rheumatology and was started on azathioprine monotherapy in the hope this would offer disease- modifying adjuvant therapy.
In the years since diagnosis, she has continued to require frequent endoscopic procedures, though after the initiation of azathioprine, the interval between surgical interventions has steadily increased.

In the future, if her disease should progress or fail to respond to systemic therapy and endoscopic treatment, then surgical resection of the entire involved segment may be required.
References and suggested readings:
Gelbard A, Donovan DT, Ongkasuwan J, et al. Disease homogeneity and treatment heterogeneity in idiopathic subglottic stenosis. Laryngoscope. 2016;126(6):1390-1396.
Mark EJ, Meng F, Kradin RL, et al. Idiopathic tracheal stenosis: a clinicopathologic study of 63 cases and comparison of the pathology with chondromalacia. Am J Surg Pathol. 2008;32(8):1138-1143.
Blumin JH, Johnston N. Evidence of extraesophageal reflux in idiopathic subglottic stenosis. Laryngoscope. 2011;121(6):1266-1273.
Gelbard A, Katsantonis NG, Mizuta M, et al. Molecular analysis of idiopathic subglottic stenosis for Mycobacterium species. Laryngoscope. 2017;127(1): 179-185.