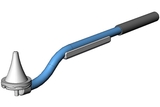
A multidisciplinary team at CHOP, composed of pediatric urologist Jason Van Batavia, MD, MSTR, nurse practitioner Joy C. Kerr, DNP, CPNP-PC, CRNFA and occupational therapist Michelle Hsia, MS, OTR/L, developed a tool to assist children with neurologic conditions leading to bowel incontinence. This tool, called the Indepenema, is a handheld device that allows patients to independently administer a cone enema and improves the associated process.
Who is Indepenema for?
Children with neurologic conditions like spinal cord injury (SCI), multiple sclerosis (MS) and spina bifida (SB) may have damage to the nerves that innervate the bowel, leading to difficulty having bowel movements and stool leakage (neurogenic bowel). While approximately 0.3-5.0% of the general population is estimated to have neurogenic bowel, the majority of patients with spina bifida have or will develop neurogenic bowel in childhood.
SB refers to one of several conditions involving neural tube birth defects that occur when the spine and the spinal cord form improperly. Patients with SB suffer from spinal deformities, visual motor impairments, lower extremity impairment, challenges with bowel and bladder function, and poor trunk strength and stability. Approximately 80% of SB patients with neurogenic bowel require intrusive options including daily high-volume enemas.
Why patients needed a new tool
While high-volume daily enemas can help children with SB achieve bowel continence, they require the assistance of another person, such as a caregiver, to administer the cone enema, severely limiting independence. Current standards of care do not address issues with the cone enema systems, nor do they consider improvements in quality of life for these patients.
Improving early independence in pediatric patients has a profound positive impact on children’s social development, participation with peers, educational engagement and overall life trajectory. Most importantly it helps transition patients into independent adults. This type of intervention at an early age can significantly impact the patient’s and the family's quality of life.
How Indepenema was developed

The development of this device started as a napkin drawing and early prototype from supplies in the occupational therapy (OT) office, then moved to initial funding and support by CHOP’s Office of Entrepreneurship and Innovation (OEI). OEI was established to accelerate innovative ideas from CHOP faculty and staff that promise commercialization. OEI receives 100 applications on average per year and accepts about five new projects to provide seed funding. When the clinical team’s device was selected, a project manager was assigned to help guide them through the biodesign process. Next, the team met with several local medical manufacturing companies, selected CAD designs, made iterative adjustments and produced a working prototype!
With ten prototypes in hand, the clinical team developed a protocol for the first-in-human study. After clearance by the CHOP Medical Device Committee and Internal Review Board (IRB), the Indepenema pilot study was initiated and completed over a 6-month period. The success of this feasibility trial at CHOP and the direct patient and family feedback received led to further refinements to the working prototype. Several patients and families noted that with slight improvements the device could drastically change their lives. This iterative process with direct patient/consumer feedback has led to the development of a new prototype that will be studied in the upcoming year.
During this process, additional support and funding was provided by the FDA Southwest National Pediatric Device Innovation Consortium (SWPDC), American Academy of Pediatrics Device Prize and the CHOP Women’s Committee.
A multidisciplinary team at CHOP, composed of pediatric urologist Jason Van Batavia, MD, MSTR, nurse practitioner Joy C. Kerr, DNP, CPNP-PC, CRNFA and occupational therapist Michelle Hsia, MS, OTR/L, developed a tool to assist children with neurologic conditions leading to bowel incontinence. This tool, called the Indepenema, is a handheld device that allows patients to independently administer a cone enema and improves the associated process.
Who is Indepenema for?
Children with neurologic conditions like spinal cord injury (SCI), multiple sclerosis (MS) and spina bifida (SB) may have damage to the nerves that innervate the bowel, leading to difficulty having bowel movements and stool leakage (neurogenic bowel). While approximately 0.3-5.0% of the general population is estimated to have neurogenic bowel, the majority of patients with spina bifida have or will develop neurogenic bowel in childhood.
SB refers to one of several conditions involving neural tube birth defects that occur when the spine and the spinal cord form improperly. Patients with SB suffer from spinal deformities, visual motor impairments, lower extremity impairment, challenges with bowel and bladder function, and poor trunk strength and stability. Approximately 80% of SB patients with neurogenic bowel require intrusive options including daily high-volume enemas.
Why patients needed a new tool
While high-volume daily enemas can help children with SB achieve bowel continence, they require the assistance of another person, such as a caregiver, to administer the cone enema, severely limiting independence. Current standards of care do not address issues with the cone enema systems, nor do they consider improvements in quality of life for these patients.
Improving early independence in pediatric patients has a profound positive impact on children’s social development, participation with peers, educational engagement and overall life trajectory. Most importantly it helps transition patients into independent adults. This type of intervention at an early age can significantly impact the patient’s and the family's quality of life.
How Indepenema was developed

The development of this device started as a napkin drawing and early prototype from supplies in the occupational therapy (OT) office, then moved to initial funding and support by CHOP’s Office of Entrepreneurship and Innovation (OEI). OEI was established to accelerate innovative ideas from CHOP faculty and staff that promise commercialization. OEI receives 100 applications on average per year and accepts about five new projects to provide seed funding. When the clinical team’s device was selected, a project manager was assigned to help guide them through the biodesign process. Next, the team met with several local medical manufacturing companies, selected CAD designs, made iterative adjustments and produced a working prototype!
With ten prototypes in hand, the clinical team developed a protocol for the first-in-human study. After clearance by the CHOP Medical Device Committee and Internal Review Board (IRB), the Indepenema pilot study was initiated and completed over a 6-month period. The success of this feasibility trial at CHOP and the direct patient and family feedback received led to further refinements to the working prototype. Several patients and families noted that with slight improvements the device could drastically change their lives. This iterative process with direct patient/consumer feedback has led to the development of a new prototype that will be studied in the upcoming year.
During this process, additional support and funding was provided by the FDA Southwest National Pediatric Device Innovation Consortium (SWPDC), American Academy of Pediatrics Device Prize and the CHOP Women’s Committee.