Christina L. Szperka, MD, MSCE, Director, Pediatric Headache Program
Case: KR is a 5-year-old girl with a history of asthma who presents to your office for recurrent headaches. Parents report the child has episodes approximately 2 times per month. There was no significant change in her medical or social history around the time these episodes started, and the pattern has been stable for the last 6 months.
They come in today because she had an episode at school, and the teacher was concerned. Sometimes episodes seem to be triggered by dehydration, excitement, staying up late, or stressors. Though she is reluctant to answer your questions, her parents report that during the episodes she stops playing, rubs her forehead, asks her siblings to be quiet, and tries to cover her eyes.
Within a half hour she looks pale and sometimes vomits. She sleeps for a little while then seems much better when she awakens. Episodes can occur at any time of day. When you ask about family history, dad reports he sometimes got sinus headaches and mom has had headaches with menses since her teenage years. Neither have ever sought medical care for headache.
Discussion: Headache is a very common symptom, affecting about 60% of children globally. Recurrent headaches cause substantial disability and lower quality of life. While we often worry that headache is a symptom of dangerous conditions like brain tumor, thankfully that is rare. Life-threatening causes occur in ~1% of children with headache who present to primary care. The first step in approaching patients with headache is to consider if the history fits with a secondary headache, where headache is a symptom of another problem, or a primary headache disorder. Most secondary headaches in children are caused by mild infections, like colds and flu. Sometimes there’s a mix of both, as mild infections can trigger a flare of migraine in a child who also has recurrent headaches. Information to help with diagnosis of primary vs. secondary headache and treatment of primary headache disorders can be found in the new Primary Care Clinical Pathway for Management and Evaluation of Child with Headache, available at www.chop.edu/pathways.
Worrisome Symptoms?
KR’s symptoms as described are consistent with migraine. Migraine occurs in about 9% of children, with equal predominance in young boys and girls, becoming much more common in teenage girls, especially after puberty.
There is often a family history of headaches, even if family members didn’t receive a migraine diagnosis. Though young children may not be able to report their symptoms directly, attacks can come on quickly, with caregiver-observed photophobia and phonophobia, as well as vomiting.
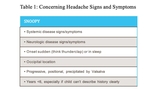
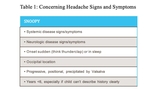
While KR is on the young side, her symptoms are consistent with migraine. The chronic, nonprogressive pattern of attacks is very reassuring. To review the signs and symptoms of worrisome cause of headache, use the mnemonic SNOOPY. (See Table 1). Most worrisome are headaches accompanied by persistent confusion or altered consciousness, new seizures, severe and abrupt thunderclap onset, meningeal sings, abnormal neurological exam, or symptoms of increased intracranial pressure. These signs/symptoms should prompt referral to the Emergency Department. If KR’s neurological exam, including fundoscopic exam, is normal, it would be appropriate to diagnose her with migraine.
Treatment: Three Parts
Treatment of primary headaches includes 3 parts. First, SMART habits encourage regular Sleep, Meals, Activity, Relaxation, and avoidance of Triggers. For example, taking a water bottle to school can keep kids hydrated. Second, acute attacks should be treated as soon as symptoms start. First line is usually ibuprofen ~10mg/kg at onset. If that’s insufficient, additional acute treatments such as anti-emetics (metoclopramide or ondansetron) or triptans (such as rizatriptan, which is FDA-approved for ages 6+) can be added. Finally, if KR were having attacks at least once per week or missing a lot of school, preventive supplements such as magnesium and riboflavin could be tried.
Steps for PCPs
If headache comes up in the context of a well visit, consider scheduling a separate visit to explore history and symptoms more thoroughly.
For a patient with symptoms concerning for secondary headache, but nothing so worrisome as to prompt ED evaluation, consider non-urgent outpatient brain MRI. Alternately, schedule a follow-up to see if there is any evolution of symptoms or if symptoms improve with SMART treatment. Approximately three-fourths of outpatient care for migraine in children is delivered by pediatricians or family physicians.
For children with unusual headaches, and children who are not improving with first-line treatments, a general pediatric Neurology consult is appropriate. Information to help with diagnosis of primary vs. secondary headache and treatment of primary headache disorders can be found in the new Primary Care Clinical Pathway for Management and Evaluation of Child with Headache.
References and Suggested Readings
Abu-Arafeh I, Razak S, Sivaraman B, Graham C. Prevalence of headache and migraine in children and adolescents: a systematic review of population-based studies. Dev Med Child Neurol. 2010;52(12):1088-1097.
Wober-Bingol C, Wober C, Uluduz D, et al. The global burden of headache in children and adolescents - developing a questionnaire and methodology for a global study. Journal Headache Pain. 2014;15:86.
Turner SB, Szperka CL, Hershey AD, et al. Association of headache with school functioning among children and adolescents in the United States. JAMA Pediatrics. 2021;175(5):522-524.
Powers SW, Patton SR, Hommel KA, et al. Quality of life in childhood migraines: clinical impact and comparison to other chronic illnesses. Pediatrics. 2003;112(1 Pt 1):e1-5.
Kernick D, Stapley S, Campbell J, et al. What happens to new-onset headache in children that present to primary care? A case-cohort study using electronic primary care records. Cephalalgia. 2009;29(12):1311-1316.
Szperka C. Headache in Children and Adolescents. Continuum (Minneapolis, Minn). 2021;27(3):703-731.
Gelfand AA, Irwin SL. Lifestyle advice for pediatric migraine: blaming the patient, or evidence based? Semin Neurol. 2020;40(3):277-285.
Lai LL, Koh L, Ho JA, et al. Off-label prescribing for children with migraines in U.S. ambulatory care settings. J Managed Care Spec Pharm. 2017;23(3):382-387.
Featured in this article
Specialties & Programs
Christina L. Szperka, MD, MSCE, Director, Pediatric Headache Program
Case: KR is a 5-year-old girl with a history of asthma who presents to your office for recurrent headaches. Parents report the child has episodes approximately 2 times per month. There was no significant change in her medical or social history around the time these episodes started, and the pattern has been stable for the last 6 months.
They come in today because she had an episode at school, and the teacher was concerned. Sometimes episodes seem to be triggered by dehydration, excitement, staying up late, or stressors. Though she is reluctant to answer your questions, her parents report that during the episodes she stops playing, rubs her forehead, asks her siblings to be quiet, and tries to cover her eyes.
Within a half hour she looks pale and sometimes vomits. She sleeps for a little while then seems much better when she awakens. Episodes can occur at any time of day. When you ask about family history, dad reports he sometimes got sinus headaches and mom has had headaches with menses since her teenage years. Neither have ever sought medical care for headache.
Discussion: Headache is a very common symptom, affecting about 60% of children globally. Recurrent headaches cause substantial disability and lower quality of life. While we often worry that headache is a symptom of dangerous conditions like brain tumor, thankfully that is rare. Life-threatening causes occur in ~1% of children with headache who present to primary care. The first step in approaching patients with headache is to consider if the history fits with a secondary headache, where headache is a symptom of another problem, or a primary headache disorder. Most secondary headaches in children are caused by mild infections, like colds and flu. Sometimes there’s a mix of both, as mild infections can trigger a flare of migraine in a child who also has recurrent headaches. Information to help with diagnosis of primary vs. secondary headache and treatment of primary headache disorders can be found in the new Primary Care Clinical Pathway for Management and Evaluation of Child with Headache, available at www.chop.edu/pathways.
Worrisome Symptoms?
KR’s symptoms as described are consistent with migraine. Migraine occurs in about 9% of children, with equal predominance in young boys and girls, becoming much more common in teenage girls, especially after puberty.
There is often a family history of headaches, even if family members didn’t receive a migraine diagnosis. Though young children may not be able to report their symptoms directly, attacks can come on quickly, with caregiver-observed photophobia and phonophobia, as well as vomiting.
While KR is on the young side, her symptoms are consistent with migraine. The chronic, nonprogressive pattern of attacks is very reassuring. To review the signs and symptoms of worrisome cause of headache, use the mnemonic SNOOPY. (See Table 1). Most worrisome are headaches accompanied by persistent confusion or altered consciousness, new seizures, severe and abrupt thunderclap onset, meningeal sings, abnormal neurological exam, or symptoms of increased intracranial pressure. These signs/symptoms should prompt referral to the Emergency Department. If KR’s neurological exam, including fundoscopic exam, is normal, it would be appropriate to diagnose her with migraine.
Treatment: Three Parts
Treatment of primary headaches includes 3 parts. First, SMART habits encourage regular Sleep, Meals, Activity, Relaxation, and avoidance of Triggers. For example, taking a water bottle to school can keep kids hydrated. Second, acute attacks should be treated as soon as symptoms start. First line is usually ibuprofen ~10mg/kg at onset. If that’s insufficient, additional acute treatments such as anti-emetics (metoclopramide or ondansetron) or triptans (such as rizatriptan, which is FDA-approved for ages 6+) can be added. Finally, if KR were having attacks at least once per week or missing a lot of school, preventive supplements such as magnesium and riboflavin could be tried.
Steps for PCPs
If headache comes up in the context of a well visit, consider scheduling a separate visit to explore history and symptoms more thoroughly.
For a patient with symptoms concerning for secondary headache, but nothing so worrisome as to prompt ED evaluation, consider non-urgent outpatient brain MRI. Alternately, schedule a follow-up to see if there is any evolution of symptoms or if symptoms improve with SMART treatment. Approximately three-fourths of outpatient care for migraine in children is delivered by pediatricians or family physicians.
For children with unusual headaches, and children who are not improving with first-line treatments, a general pediatric Neurology consult is appropriate. Information to help with diagnosis of primary vs. secondary headache and treatment of primary headache disorders can be found in the new Primary Care Clinical Pathway for Management and Evaluation of Child with Headache.
References and Suggested Readings
Abu-Arafeh I, Razak S, Sivaraman B, Graham C. Prevalence of headache and migraine in children and adolescents: a systematic review of population-based studies. Dev Med Child Neurol. 2010;52(12):1088-1097.
Wober-Bingol C, Wober C, Uluduz D, et al. The global burden of headache in children and adolescents - developing a questionnaire and methodology for a global study. Journal Headache Pain. 2014;15:86.
Turner SB, Szperka CL, Hershey AD, et al. Association of headache with school functioning among children and adolescents in the United States. JAMA Pediatrics. 2021;175(5):522-524.
Powers SW, Patton SR, Hommel KA, et al. Quality of life in childhood migraines: clinical impact and comparison to other chronic illnesses. Pediatrics. 2003;112(1 Pt 1):e1-5.
Kernick D, Stapley S, Campbell J, et al. What happens to new-onset headache in children that present to primary care? A case-cohort study using electronic primary care records. Cephalalgia. 2009;29(12):1311-1316.
Szperka C. Headache in Children and Adolescents. Continuum (Minneapolis, Minn). 2021;27(3):703-731.
Gelfand AA, Irwin SL. Lifestyle advice for pediatric migraine: blaming the patient, or evidence based? Semin Neurol. 2020;40(3):277-285.
Lai LL, Koh L, Ho JA, et al. Off-label prescribing for children with migraines in U.S. ambulatory care settings. J Managed Care Spec Pharm. 2017;23(3):382-387.
Contact us
Pediatric Headache Program