Gastroparesis is a complex gastrointestinal motility disorder characterized by delayed emptying of gastric contents in the absence of mechanical obstruction. The different portions of the stomach perform different actions: (a). Fundus — gastric accommodation by relaxation of fundus, (b). Corpus — mixing with gastric enzymes and acid, (c). Antrum — circumferential contractions to help break down the food into small particles and (d). Antro-duodenal coordination — to help empty food into the duodenum2. Any impairment of these gastric functions can result in gastroparesis.
Epidemiology and etiopathogenesis: The true prevalence of this debilitating illness in pediatrics is unknown, but recent data has shown increase in rate of hospitalizations from gastroparesis, along with increased health costs, up to 6 fold over the last few years. In children, the most common cause of gastroparesis is idiopathic; other causes include post-viral, post-surgical, and related to medications.
Clinical presentation, diagnosis, and treatment: Gastroparesis symptoms vary based on age of presentation. Younger children present with vomiting, and elder children present with nausea and abdominal pain. Other symptoms include early satiety, bloating, failure to thrive, and weight loss.
It is important to note that diagnosis of gastroparesis is challenging due to paucity of data in pediatrics. However, the best approach to diagnosis is a milk scan in younger kids and a 4-hour solid meal gastric emptying scan in elder kids. For refractory gastroparesis at Children's Hospital of Philadelphia (CHOP), we perform antroduodenal manometry testing to understand the stomach and small bowel motility.
In general, the treatment for gastroparesis is of three folds:
- dietary manipulation (gastroparesis diet: low fat/fiber diet and small frequent meals)
- medications, including cyproheptadine (improves gastric accommodation) and promotility agents like erythromycin, azithromycin, metoclopramide, domperidone or cisapride (improves gastric motility)
- addressing psychosocial issues with the support of GI psychology
Advanced diagnostics and treatment modalities: At CHOP, in our Suzi and Scott Lustgarten Center for GI Motility, we have a comprehensive, well-rounded team that includes pediatric gastroenterologists with specialized training in neurogastroenterology and motility disorders, nurse practitioners, GI psychologists, dietician, nurses, and social workers who provide a comprehensive clinic visit for evaluation and treatment of children with gastroparesis.
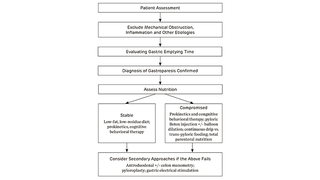
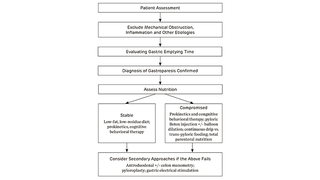
Our approach to gastroparesis is laid out in Figure 1, which is based on a recently published review article on gastroparesis in pediatrics. This approach has been endorsed by the American Neurogasteroenterology and Motility Society. Advanced diagnostics for gastroparesis available at CHOP include wireless motility capsule to assess transit time, EndoFLIP® to assess pyloric distensibility, and high-resolution electrogastrography (HR-EGG). CHOP is the first pediatric center to use EndoFLIP in gastroparesis in pediatrics as a method to understand the pyloric distensibility in gastroparesis and to help predict success of treatment outcomes. HR-EGG is a noninvasive method of mapping spatial abnormalities of gastric slow wave in children with gastroparesis, a technique pioneered by center director Hayat Mousa, MD.
Advanced treatment options available at CHOP include options to do specific drugs like domperidone and cisapride, which are available through our specially approved research protocols. For refractory gastroparesis, as an alternative to medications we perform intra-pyloric botulinum injections. In addition, we plan to launch a center for gastric electric stimulation in the near future with the expertise of Mousa. Gastric electric stimulation has shown promising results in the treatment of gastroparesis in children and adolescents.
Our mission at the Suzi and Scott Lustgarten Motility Center is to help every child referred to with gastroparesis, and we want to make this positive change in partnership with the families, primary care doctors, and specialists in the community. Learn more about the center, including family stories of children who have been treated successfully there.
Figure 1
Approach to Gastroparesis in the Suzi and Scott Lustgarten Motility Center. Adapted from: Kovacic K, Elfar W, Rosen JM, et al. Update on pediatric gastroparesis: A review of the published literature and recommendations for future research. Neurogastroenterol Motil. 2020;32(3).
References and Further Readings
Camilleri M, Parkman HP, Shafi MA, et al. Clinical guideline: management of gastroparesis. American College of Gastroenterology. Am J Gastroenterol. 2013;108(1):18-37.
Lu PL, Moore-Clingenpeel M, Yacob D, Di Lorenzo C, Mousa HM. The rising cost of hospital care for children with gastroparesis: 2004-2013. Neurogastroenterol Motil. 2016;28(11):1698-1704.
Edwards ST, Cocjin J, Theut SB, et al. A comparison of the diagnosis of gastroparesis in 4 h pediatric gastric emptying studies versus 2 h studies. BMC Gastroenterol. 2019; 19(1):26.
Gharibans AA, Coleman TP, Mousa H, Kunkel DC. Spatial patterns from high-resolution electrogastrography correlate with severity of symptoms in patients with functional dyspepsia and gastroparesis. Clin Gastroenterol Hepatol. 2019;17(13):2668-2677.
Teich S, Mousa HM, Punati J, Di Lorenzo C. Efficacy of permanent gastric electrical stimulation for the treatment of gastroparesis and functional dyspepsia in children and adolescents. J Pediatr Surg. 2013;48(1):178-83.
Featured in this article
Specialties & Programs
Gastroparesis is a complex gastrointestinal motility disorder characterized by delayed emptying of gastric contents in the absence of mechanical obstruction. The different portions of the stomach perform different actions: (a). Fundus — gastric accommodation by relaxation of fundus, (b). Corpus — mixing with gastric enzymes and acid, (c). Antrum — circumferential contractions to help break down the food into small particles and (d). Antro-duodenal coordination — to help empty food into the duodenum2. Any impairment of these gastric functions can result in gastroparesis.
Epidemiology and etiopathogenesis: The true prevalence of this debilitating illness in pediatrics is unknown, but recent data has shown increase in rate of hospitalizations from gastroparesis, along with increased health costs, up to 6 fold over the last few years. In children, the most common cause of gastroparesis is idiopathic; other causes include post-viral, post-surgical, and related to medications.
Clinical presentation, diagnosis, and treatment: Gastroparesis symptoms vary based on age of presentation. Younger children present with vomiting, and elder children present with nausea and abdominal pain. Other symptoms include early satiety, bloating, failure to thrive, and weight loss.
It is important to note that diagnosis of gastroparesis is challenging due to paucity of data in pediatrics. However, the best approach to diagnosis is a milk scan in younger kids and a 4-hour solid meal gastric emptying scan in elder kids. For refractory gastroparesis at Children's Hospital of Philadelphia (CHOP), we perform antroduodenal manometry testing to understand the stomach and small bowel motility.
In general, the treatment for gastroparesis is of three folds:
- dietary manipulation (gastroparesis diet: low fat/fiber diet and small frequent meals)
- medications, including cyproheptadine (improves gastric accommodation) and promotility agents like erythromycin, azithromycin, metoclopramide, domperidone or cisapride (improves gastric motility)
- addressing psychosocial issues with the support of GI psychology
Advanced diagnostics and treatment modalities: At CHOP, in our Suzi and Scott Lustgarten Center for GI Motility, we have a comprehensive, well-rounded team that includes pediatric gastroenterologists with specialized training in neurogastroenterology and motility disorders, nurse practitioners, GI psychologists, dietician, nurses, and social workers who provide a comprehensive clinic visit for evaluation and treatment of children with gastroparesis.
Our approach to gastroparesis is laid out in Figure 1, which is based on a recently published review article on gastroparesis in pediatrics. This approach has been endorsed by the American Neurogasteroenterology and Motility Society. Advanced diagnostics for gastroparesis available at CHOP include wireless motility capsule to assess transit time, EndoFLIP® to assess pyloric distensibility, and high-resolution electrogastrography (HR-EGG). CHOP is the first pediatric center to use EndoFLIP in gastroparesis in pediatrics as a method to understand the pyloric distensibility in gastroparesis and to help predict success of treatment outcomes. HR-EGG is a noninvasive method of mapping spatial abnormalities of gastric slow wave in children with gastroparesis, a technique pioneered by center director Hayat Mousa, MD.
Advanced treatment options available at CHOP include options to do specific drugs like domperidone and cisapride, which are available through our specially approved research protocols. For refractory gastroparesis, as an alternative to medications we perform intra-pyloric botulinum injections. In addition, we plan to launch a center for gastric electric stimulation in the near future with the expertise of Mousa. Gastric electric stimulation has shown promising results in the treatment of gastroparesis in children and adolescents.
Our mission at the Suzi and Scott Lustgarten Motility Center is to help every child referred to with gastroparesis, and we want to make this positive change in partnership with the families, primary care doctors, and specialists in the community. Learn more about the center, including family stories of children who have been treated successfully there.
Figure 1
Approach to Gastroparesis in the Suzi and Scott Lustgarten Motility Center. Adapted from: Kovacic K, Elfar W, Rosen JM, et al. Update on pediatric gastroparesis: A review of the published literature and recommendations for future research. Neurogastroenterol Motil. 2020;32(3).
References and Further Readings
Camilleri M, Parkman HP, Shafi MA, et al. Clinical guideline: management of gastroparesis. American College of Gastroenterology. Am J Gastroenterol. 2013;108(1):18-37.
Lu PL, Moore-Clingenpeel M, Yacob D, Di Lorenzo C, Mousa HM. The rising cost of hospital care for children with gastroparesis: 2004-2013. Neurogastroenterol Motil. 2016;28(11):1698-1704.
Edwards ST, Cocjin J, Theut SB, et al. A comparison of the diagnosis of gastroparesis in 4 h pediatric gastric emptying studies versus 2 h studies. BMC Gastroenterol. 2019; 19(1):26.
Gharibans AA, Coleman TP, Mousa H, Kunkel DC. Spatial patterns from high-resolution electrogastrography correlate with severity of symptoms in patients with functional dyspepsia and gastroparesis. Clin Gastroenterol Hepatol. 2019;17(13):2668-2677.
Teich S, Mousa HM, Punati J, Di Lorenzo C. Efficacy of permanent gastric electrical stimulation for the treatment of gastroparesis and functional dyspepsia in children and adolescents. J Pediatr Surg. 2013;48(1):178-83.
Contact us
Suzi and Scott Lustgarten Center for GI Motility