
In October 2019, N. Scott Adzick, MD, Surgeon-in-Chief of Children’s Hospital of Philadelphia and the founder and Director of the Center for Fetal Diagnosis and Treatment, presented the Tower Lecture at the 38th meeting of the International Fetal Medicine and Surgery Society in Sils, Engadin, Switzerland. The topic was presented in three parts as an oral presentation: Fetal Surgery Past, Fetal Surgery Present, and Fetal Surgery Yet to Come! Read on for a glimpse into what shaped the field of fetal surgery, and what the future holds.
This article is posted with permission from Fetal Diagnosis and Therapy, where it was published online on Sept. 2, 2020.
Introduction

The Tower Lecture was given at the 38th meeting of the International Fetal Medicine and Surgery Society in Sils-Maria, Engadin, Switzerland, on October 25, 2019. The topic was presented in three parts: Fetal Surgery Past, Fetal Surgery Present, and Fetal Surgery Yet to Come! The venue for the Tower Lecture was the magnificent Tower at 2,284 m altitude, located within the historic Julier Pass, a crucial north-south passageway within the Swiss Alps, and a watershed area for the Rivers Danube, Rhine, and Po. Inspiring musical performances were provided before, between, and after the three parts of the Tower Lecture by the Incantanti who were fantastically animated singers and performers under Musical Director Christian Klucker.
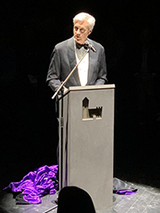
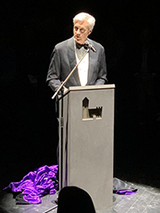
I am the Prince of the Tower (Fig. 1), here to tell you riveting tales equal to the fabulous iconography of this magnificent place (Fig. 2) – stories of Fetal Surgery Past, Fetal Surgery Present, and Fetal Surgery Yet to Come!

Fig. 2: The venue for the Tower Lecture was the magnificent Tower at 2,284 m altitude, located within the historic Julier Pass, a crucial north-south passageway within the Swiss Alps, and a watershed area for the Rivers Danube, Rhine, and Po. A, The tower by day. B, The tower by night.
Fetal Surgery Past: In the Beginning…
For most of human history, the fetus was shrouded in mystery, hidden away inside the pregnant mother as a medical recluse. Historically, the Greek and Roman philosophers conceived the idea of the homunculus – a miniature person living and growing within the mother before birth. In 16th century Padua, Italy, the great anatomist Andreas Vesalius performed the first truly anatomic observations on the mammalian fetus. At the same time, half a world away, the Incas of Peru crafted pottery depicting a variety of birth defects, ranging from facial clefts to massive hydrocephalus to conjoined twins. The fetus became a patient for the first time in 1961, when Sir William Liley, blindly – and successfully – performed intrauterine blood transfusion into the fetal abdomen to treat otherwise fatal erythroblastosis fetalis. To quote Claudius in Shakespeare’s Hamlet: “Diseases desperate grown, by desperate means are relieved… Or not at all.” In the 1970s, experience with ultrasound technology and other prenatal diagnostic techniques led to the accurate diagnosis before birth of many anatomic and genetic defects. In the 1980s, the rationale and feasibility of in utero repair for various life-threatening anomalies was explored arising from the clinical frustration in caring for newborn babies with problems that were “too late to correct,” if only we had gotten to the problem earlier, that is before birth.
The earthquake epicenter for the development of fetal surgery was the University of California San Francisco, and the leader was the one-of-a-kind creative genius, Michael Richard Harrison. I walked into Mike Harrison’s “hole in the wall” laboratory at UCSF as a surgical research fellow in July 1983, soon to be joined by the not-yet-world-famous Alan Flake, and with time we were fortuitously flooded with a tsunami of bright, ambitious, and resourceful research fellows. We did fetal sheep surgery in a Q-fever quarantined facility at UCSF dubbed “Sheepland” where investigators had to wear bright orange jumpsuits similar to those worn by prisoners in the high-security San Quentin Penitentiary. We transported still anesthetized postoperative pregnant maternal sheep from the Operating Room to their Recovery Pens in a specially constructed cart called the “Lamb-ulance.” We took many “roadtrips” to the California Primate Research Center in Davis, California, to operate on time-dated pregnant rhesus monkeys. In 1984, while a research fellow, I created a big Fame-o-Meter poster with a scale: Nobel Prize at the top, and at the bottom of the scale was an airplane in flames – “crashing and burning.”
At the end of each day, the laboratory technicians would grade us on how we had done with our experiments: mostly “crash and burn,” but there were a few blips of success registered on the Fame-o-Meter. Figure 3 shows the wallet-size version of the Fame-o-Meter in case you would like to see it. Over the next decade, many fetal surgical principles were developed, such as the invention of the uterine stapling device, from more than 1,600 operations in fetal lambs and more than 400 operations in fetal rhesus monkeys.
The crucial organization that fostered the development of fetal surgery was the International Fetal Medicine and Surgery Society (IFMSS), springing from a symposium that Mike Harrison organized in Santa Barbara, California, in 1982 at the Kroc Foundation Ranch. The Kroc Foundation is the philanthropic limb of the McDonald’s Corporation – that’s right, all of our work was initially launched from hamburgers and French fries! From that conference, a New England Journal of Medicine position statement emerged about invasive fetal therapy, and an International Fetal Treatment Registry was established. The principles or “rules to live by” came from the open and frank discussions at many IFMSS meetings. We recognized that fetal surgery should only be considered in centers that are committed to a program of continuing research together with cautious clinical application. We recommended that a fetal treatment center requires the close collaboration of dedicated pediatric surgeons, maternal-fetal medicine specialists, sonographers, echocardiographers, neonatologists, geneticists, ethicists, neonatal and obstetric nurses, and a compassionate nurse coordinator, who all “rub shoulders” to cooperatively address prenatally diagnosed problems. We agreed that the fetal treatment team should be committed to having this innovative therapy reviewed by uninvolved professional colleagues (Institutional Review Board and/or fetal therapy oversight committee), to publish all results (bad as well as good), to avoid media reports until cases are peer reviewed, and to test the validity and cost-effectiveness of this approach in properly controlled trials. The journal Fetal Diagnosis and Therapy arose from these discussions as the official voice of the IFMSS.
Contributions from many centers presented at the IFMSS during the late 20th century included the following.
Use of double pig-tail catheter vesicoamniotic shunts to decompress obstructed fetal urinary bladders, as well as thoracoamniotic shunts to treat cystic lung disease and pleural effusions associated with fetal hydrops.
In contrast, a moratorium was recommended by the IFMSS on the use of fetal shunts to treat progressive hydrocephalus due to inadequacies in diagnosis, ineffective shunting techniques, and improper selection criteria.
There was successful in utero resection of lung lesions and sacrococcygeal teratomas in hydropic fetuses.
There was successful fetoscopic laser ablation of abnormal shared placental vessels to treat twin-twin transfusion syndrome (TTTS).
Open fetal surgical repair of congenital diaphragmatic hernia (CDH) was tested and then abandoned because the most severely affected fetuses have liver herniation, and liver reduction into the fetal abdomen compromised umbilical blood flow. Fetal tracheal occlusion was then tried to enhance fetal lung growth in these severe cases, and “deplugging” the trachea later in gestation spawned the concept of ex utero intrapartum therapy or the EXIT procedure, which was subsequently used worldwide for extrinsic fetal airway obstruction (due to giant fetal neck masses) or intrinsic fetal airway obstruction (congenital high airway obstruction syndrome – CHAOS) and for other indications.
Fetal surgery in the 21st century was about to blossom (Fig. 4).

Fig.4: Inspiring musical performances were provided before, between, and after the three parts of the Tower Lecture. A, Musical Director Christian Klucker with the Incantanti. B, The Incantanti were fantastically animated singers and performers.
Fetal Surgery Present: Trials, Tribulations, and Collaborations
The current era in the early 21st century is characterized by the move from clinical descriptions and retrospective analyses to randomized controlled trials.
The Eurofetus randomized trial showed the superiority of fetoscopic laser photocoagulation compared to amniodrainage for twin-twin transfusion syndrome (TTTS). Now, further refinement of indications, instrumentation, and techniques are in play including the treatment of many other “troubles with twins” as we have heard at this IFMSS meeting.
Martin and Claudia Meuli developed the fetal lamb spina bifida model, confirmed the two-hit hypothesis, and showed that in utero repair could prevent further neurological damage – work published in Nature Medicine. The road to the Management of Myelomeningocele Study – the MOMS trial – was long and difficult, and entailed a philosophical change for fetal surgery: from treating only life-threatening birth defects to treating devastating birth defects that are not truly life-or-death. At the IFMSS meeting on Nantucket in 2000, commitments to the MOMS trial were made by the 3 centers (UCSF, Vanderbilt, CHOP), and an agreement was forged that other interested centers would not “backdoor” fetal spina bifida surgery outside of the randomized controlled trial. The successful completion of the MOMS trial led to a NEJM publication, and thereafter generated many follow-up studies including the 35 presentations about fetal spina bifida at this IFMSS conference. An NIH-sponsored task force issued guidelines for institutional criteria to perform fetal spina bifida repair. Thereafter, there has been an explosive growth in fetal surgery centers worldwide, which has catalyzed efforts for “how to train teams.” Ongoing dramatic improvements in results have occurred since the first MOMS trial publication 8 years ago. Minimally invasive fetoscopic approaches for fetal spina bifida repair show promise to decrease maternal morbidity if the results for the baby prove to be comparable to those of open repair.
There have been other moves from open fetal surgery to less invasive approaches – here are two examples. First, the treatment of fetal CDH with single port fetal endoscopic tracheal occlusion (FETO) and now the TOTAL trial (Tracheal Occlusion to Accelerate Lung growth) is underway. The “moderate” limb of the trial is now closed to enrollment and we await the results to be revealed in 2020! The “severe” limb of the trial is ongoing. Second, the move from open fetal resection of lung lesions associated with hydrops – now a rare fetal surgery – to successful treatment with one or more courses of maternal betamethasone. Remarkable!
Catheter-based fetal cardiac interventions such as valvuloplasty for aortic stenosis and pulmonic stenosis, and septoplasty for Hypoplastic Left Heart Syndrome with intact atrial septum.
Recent successful resections of fetal pericardial teratomas and mediastinal teratomas in hydropic fetuses.
Advances in imaging include the emergence of ultrafast fetal MRI to provide a new tool for the diagnosis of fetal anomalies. Better sonographic prognostic indicators have been developed, for example, cerebrovascular reactivity for fetal lung lesions, and observed-to-expected lung-to-head ratio and observed-to-expected magnetic resonance imaging lung volumes for CDH.
The first Special Delivery Unit was created in a Children’s Hospital, exclusively dedicated to the comprehensive care of the mother and fetus with a birth defect.
Collaborative fetal therapy organizations such as the North American Fetal Therapy Network (NAFTNet) founded in 2004 has now grown to 36 member centers. A powerful REDCap fetal myelomeningocele surgery registry now has more than 800 patients and thus provides scale for studies. Within NAFTNet and the IFMSS, there are now special interest groups such as for fetal therapy nurses, the diaspora generated from the leadership of Lori Howell.
Experimental work in fetal animal models is exciting – here are two highlights. The Artificial Womb developed in fetal sheep (“the lamb in a bag”), immortalized in Alan Flake’s “Bathtub Lecture” here in Sils-Maria at the European Club for Fetal Surgery in 2017, may one day provide a life-saving bridge to take premature babies safely from 23–24 weeks’ gestation with normal growth and development to 28–30 weeks’ gestation. Fetal gene therapy and in utero gene editing using CRISPR technology to treat single gene disorders now has proof of principle in fetal animal models.
Fetal Surgery Yet to Come: The Artificial Womb, Big Data, Cells, and Genes
Looking to the future, I shed my cloak, a symbolic rebirth (Fig. 5). We tend to overestimate what will happen in the next year or two, and underestimate what will be accomplished 20 years from now.
There is much more to be done, which requires research – the basis for Fetal Surgery Yet to Come. One of my teachers at Harvard Medical School and Boston Children’s Hospital, Dr. Judah Folkman, taught me that:
As long as there is an unconquered disease, an injury that cannot be repaired, or a method of prevention that remains beyond reach, we have an obligation to conduct research. Research represents HOPE, and for many patients and families, hope is the best thing we have to offer. We pursue our investigations so that one day we can offer more than HOPE, we can offer health.
As predicted in the momentous “Bathtub Lecture,” the clinical application of the artificial womb to babies born too soon at 23–24 weeks’ gestation permits continued normal growth and development for 4–5 weeks or more with dramatically better outcomes. This transformative technology in the Neonatal Intensive Care Unit of the future supporting extremely premature babies is indeed A Brave New World.
Collaboration using BIG DATA through organizations such as NAFTNet – all of us working together – will prove especially powerful to provide real-time prognostic information about birth defect outcomes, and to target the unsolved problems to overcome.
I can imagine a future state in which a mother carrying a fetus with spina bifida, diagnosed at 16 weeks’ gestation, will have the spina bifida sealed and protected before birth by injection of specific tissue-engineered components either through a fetoscope or with an ultrasound-guided amniocentesis needle, and avoid the possible complications of the big fetal surgery operations that we do now. Nature-derived tissue-engineered solutions including underwater biological glues, nanotextured biodegradable elastomers, and cell sheet technology, together with the appropriate dollop of mesenchymal stem cells or derived factors to stimulate nerve regeneration, result in enhanced motor and sensory function after fetal spina bifida repair.
Tissue-engineered solutions are crafted involving harvesting multipotent mesenchymal stem cells by amniocentesis, and then – using CDH for example – seeding muscle progenitor cells onto an acellular matrix to “grow” diaphragm for autologous diaphragmatic reconstruction after birth.
Solving the problem of membrane disruption at fetoscopic port sites permits complex minimally invasive fetal surgery procedures including the use of robotic technology.
Prenatal neuroprotection strategies improve neurodevelopmental outcomes by protecting the brain before birth – for example, in babies with complex congenital heart disease.
Whole-exome and whole-genome sequencing of the triad (mother, father, fetus) for specific birth defects sheds light on the genetic causes of those defects, and suggests therapeutic strategies for prenatal treatment.
Advances in prenatal diagnosis allows the prenatal treatment of anticipated postnatal diseases. Fetal gene therapy and in utero gene editing using prime editing with CRISPR technology are ethically applied clinically to single gene disorders and provide cures for thousands and thousands of unborn patients. A better understanding of maternal-fetal immunology makes in utero hematopoietic stem cell transplantation successful to treat cellular deficiency diseases such as sickle cell anemia, as well as other hematologic and immunologic disorders. Delineation of the immunologic “cross-talk” within the maternal-placental-fetal unit enhances our understanding and treatment of autoimmune diseases and preterm labor.
So… Fetal Surgery Yet To Come: I believe that the future is DAZZLINGLY BRIGHT (Fig. 6)!

Fig. 6: Fetal Surgery Yet to Come. Dr. Adzick holding the IFMSS Tower Lecture Award, consisting of a Julier Tower model embedded on a piece of rock from the famous Julier Pass in the Swiss Alps. He is surrounded by former pediatric and fetal surgeons who he has trained and who represent the future of the field.
Disclosure Statement
The author has no conflicts of interest to declare.
Author Contributions
Dr. N. Scott Adzick is the sole contributor to this article.
Featured in this article
Specialties & Programs
In October 2019, N. Scott Adzick, MD, Surgeon-in-Chief of Children’s Hospital of Philadelphia and the founder and Director of the Center for Fetal Diagnosis and Treatment, presented the Tower Lecture at the 38th meeting of the International Fetal Medicine and Surgery Society in Sils, Engadin, Switzerland. The topic was presented in three parts as an oral presentation: Fetal Surgery Past, Fetal Surgery Present, and Fetal Surgery Yet to Come! Read on for a glimpse into what shaped the field of fetal surgery, and what the future holds.
This article is posted with permission from Fetal Diagnosis and Therapy, where it was published online on Sept. 2, 2020.
Introduction

The Tower Lecture was given at the 38th meeting of the International Fetal Medicine and Surgery Society in Sils-Maria, Engadin, Switzerland, on October 25, 2019. The topic was presented in three parts: Fetal Surgery Past, Fetal Surgery Present, and Fetal Surgery Yet to Come! The venue for the Tower Lecture was the magnificent Tower at 2,284 m altitude, located within the historic Julier Pass, a crucial north-south passageway within the Swiss Alps, and a watershed area for the Rivers Danube, Rhine, and Po. Inspiring musical performances were provided before, between, and after the three parts of the Tower Lecture by the Incantanti who were fantastically animated singers and performers under Musical Director Christian Klucker.
I am the Prince of the Tower (Fig. 1), here to tell you riveting tales equal to the fabulous iconography of this magnificent place (Fig. 2) – stories of Fetal Surgery Past, Fetal Surgery Present, and Fetal Surgery Yet to Come!

Fig. 2: The venue for the Tower Lecture was the magnificent Tower at 2,284 m altitude, located within the historic Julier Pass, a crucial north-south passageway within the Swiss Alps, and a watershed area for the Rivers Danube, Rhine, and Po. A, The tower by day. B, The tower by night.
Fetal Surgery Past: In the Beginning…
For most of human history, the fetus was shrouded in mystery, hidden away inside the pregnant mother as a medical recluse. Historically, the Greek and Roman philosophers conceived the idea of the homunculus – a miniature person living and growing within the mother before birth. In 16th century Padua, Italy, the great anatomist Andreas Vesalius performed the first truly anatomic observations on the mammalian fetus. At the same time, half a world away, the Incas of Peru crafted pottery depicting a variety of birth defects, ranging from facial clefts to massive hydrocephalus to conjoined twins. The fetus became a patient for the first time in 1961, when Sir William Liley, blindly – and successfully – performed intrauterine blood transfusion into the fetal abdomen to treat otherwise fatal erythroblastosis fetalis. To quote Claudius in Shakespeare’s Hamlet: “Diseases desperate grown, by desperate means are relieved… Or not at all.” In the 1970s, experience with ultrasound technology and other prenatal diagnostic techniques led to the accurate diagnosis before birth of many anatomic and genetic defects. In the 1980s, the rationale and feasibility of in utero repair for various life-threatening anomalies was explored arising from the clinical frustration in caring for newborn babies with problems that were “too late to correct,” if only we had gotten to the problem earlier, that is before birth.
The earthquake epicenter for the development of fetal surgery was the University of California San Francisco, and the leader was the one-of-a-kind creative genius, Michael Richard Harrison. I walked into Mike Harrison’s “hole in the wall” laboratory at UCSF as a surgical research fellow in July 1983, soon to be joined by the not-yet-world-famous Alan Flake, and with time we were fortuitously flooded with a tsunami of bright, ambitious, and resourceful research fellows. We did fetal sheep surgery in a Q-fever quarantined facility at UCSF dubbed “Sheepland” where investigators had to wear bright orange jumpsuits similar to those worn by prisoners in the high-security San Quentin Penitentiary. We transported still anesthetized postoperative pregnant maternal sheep from the Operating Room to their Recovery Pens in a specially constructed cart called the “Lamb-ulance.” We took many “roadtrips” to the California Primate Research Center in Davis, California, to operate on time-dated pregnant rhesus monkeys. In 1984, while a research fellow, I created a big Fame-o-Meter poster with a scale: Nobel Prize at the top, and at the bottom of the scale was an airplane in flames – “crashing and burning.”
At the end of each day, the laboratory technicians would grade us on how we had done with our experiments: mostly “crash and burn,” but there were a few blips of success registered on the Fame-o-Meter. Figure 3 shows the wallet-size version of the Fame-o-Meter in case you would like to see it. Over the next decade, many fetal surgical principles were developed, such as the invention of the uterine stapling device, from more than 1,600 operations in fetal lambs and more than 400 operations in fetal rhesus monkeys.
The crucial organization that fostered the development of fetal surgery was the International Fetal Medicine and Surgery Society (IFMSS), springing from a symposium that Mike Harrison organized in Santa Barbara, California, in 1982 at the Kroc Foundation Ranch. The Kroc Foundation is the philanthropic limb of the McDonald’s Corporation – that’s right, all of our work was initially launched from hamburgers and French fries! From that conference, a New England Journal of Medicine position statement emerged about invasive fetal therapy, and an International Fetal Treatment Registry was established. The principles or “rules to live by” came from the open and frank discussions at many IFMSS meetings. We recognized that fetal surgery should only be considered in centers that are committed to a program of continuing research together with cautious clinical application. We recommended that a fetal treatment center requires the close collaboration of dedicated pediatric surgeons, maternal-fetal medicine specialists, sonographers, echocardiographers, neonatologists, geneticists, ethicists, neonatal and obstetric nurses, and a compassionate nurse coordinator, who all “rub shoulders” to cooperatively address prenatally diagnosed problems. We agreed that the fetal treatment team should be committed to having this innovative therapy reviewed by uninvolved professional colleagues (Institutional Review Board and/or fetal therapy oversight committee), to publish all results (bad as well as good), to avoid media reports until cases are peer reviewed, and to test the validity and cost-effectiveness of this approach in properly controlled trials. The journal Fetal Diagnosis and Therapy arose from these discussions as the official voice of the IFMSS.
Contributions from many centers presented at the IFMSS during the late 20th century included the following.
Use of double pig-tail catheter vesicoamniotic shunts to decompress obstructed fetal urinary bladders, as well as thoracoamniotic shunts to treat cystic lung disease and pleural effusions associated with fetal hydrops.
In contrast, a moratorium was recommended by the IFMSS on the use of fetal shunts to treat progressive hydrocephalus due to inadequacies in diagnosis, ineffective shunting techniques, and improper selection criteria.
There was successful in utero resection of lung lesions and sacrococcygeal teratomas in hydropic fetuses.
There was successful fetoscopic laser ablation of abnormal shared placental vessels to treat twin-twin transfusion syndrome (TTTS).
Open fetal surgical repair of congenital diaphragmatic hernia (CDH) was tested and then abandoned because the most severely affected fetuses have liver herniation, and liver reduction into the fetal abdomen compromised umbilical blood flow. Fetal tracheal occlusion was then tried to enhance fetal lung growth in these severe cases, and “deplugging” the trachea later in gestation spawned the concept of ex utero intrapartum therapy or the EXIT procedure, which was subsequently used worldwide for extrinsic fetal airway obstruction (due to giant fetal neck masses) or intrinsic fetal airway obstruction (congenital high airway obstruction syndrome – CHAOS) and for other indications.
Fetal surgery in the 21st century was about to blossom (Fig. 4).

Fig.4: Inspiring musical performances were provided before, between, and after the three parts of the Tower Lecture. A, Musical Director Christian Klucker with the Incantanti. B, The Incantanti were fantastically animated singers and performers.
Fetal Surgery Present: Trials, Tribulations, and Collaborations
The current era in the early 21st century is characterized by the move from clinical descriptions and retrospective analyses to randomized controlled trials.
The Eurofetus randomized trial showed the superiority of fetoscopic laser photocoagulation compared to amniodrainage for twin-twin transfusion syndrome (TTTS). Now, further refinement of indications, instrumentation, and techniques are in play including the treatment of many other “troubles with twins” as we have heard at this IFMSS meeting.
Martin and Claudia Meuli developed the fetal lamb spina bifida model, confirmed the two-hit hypothesis, and showed that in utero repair could prevent further neurological damage – work published in Nature Medicine. The road to the Management of Myelomeningocele Study – the MOMS trial – was long and difficult, and entailed a philosophical change for fetal surgery: from treating only life-threatening birth defects to treating devastating birth defects that are not truly life-or-death. At the IFMSS meeting on Nantucket in 2000, commitments to the MOMS trial were made by the 3 centers (UCSF, Vanderbilt, CHOP), and an agreement was forged that other interested centers would not “backdoor” fetal spina bifida surgery outside of the randomized controlled trial. The successful completion of the MOMS trial led to a NEJM publication, and thereafter generated many follow-up studies including the 35 presentations about fetal spina bifida at this IFMSS conference. An NIH-sponsored task force issued guidelines for institutional criteria to perform fetal spina bifida repair. Thereafter, there has been an explosive growth in fetal surgery centers worldwide, which has catalyzed efforts for “how to train teams.” Ongoing dramatic improvements in results have occurred since the first MOMS trial publication 8 years ago. Minimally invasive fetoscopic approaches for fetal spina bifida repair show promise to decrease maternal morbidity if the results for the baby prove to be comparable to those of open repair.
There have been other moves from open fetal surgery to less invasive approaches – here are two examples. First, the treatment of fetal CDH with single port fetal endoscopic tracheal occlusion (FETO) and now the TOTAL trial (Tracheal Occlusion to Accelerate Lung growth) is underway. The “moderate” limb of the trial is now closed to enrollment and we await the results to be revealed in 2020! The “severe” limb of the trial is ongoing. Second, the move from open fetal resection of lung lesions associated with hydrops – now a rare fetal surgery – to successful treatment with one or more courses of maternal betamethasone. Remarkable!
Catheter-based fetal cardiac interventions such as valvuloplasty for aortic stenosis and pulmonic stenosis, and septoplasty for Hypoplastic Left Heart Syndrome with intact atrial septum.
Recent successful resections of fetal pericardial teratomas and mediastinal teratomas in hydropic fetuses.
Advances in imaging include the emergence of ultrafast fetal MRI to provide a new tool for the diagnosis of fetal anomalies. Better sonographic prognostic indicators have been developed, for example, cerebrovascular reactivity for fetal lung lesions, and observed-to-expected lung-to-head ratio and observed-to-expected magnetic resonance imaging lung volumes for CDH.
The first Special Delivery Unit was created in a Children’s Hospital, exclusively dedicated to the comprehensive care of the mother and fetus with a birth defect.
Collaborative fetal therapy organizations such as the North American Fetal Therapy Network (NAFTNet) founded in 2004 has now grown to 36 member centers. A powerful REDCap fetal myelomeningocele surgery registry now has more than 800 patients and thus provides scale for studies. Within NAFTNet and the IFMSS, there are now special interest groups such as for fetal therapy nurses, the diaspora generated from the leadership of Lori Howell.
Experimental work in fetal animal models is exciting – here are two highlights. The Artificial Womb developed in fetal sheep (“the lamb in a bag”), immortalized in Alan Flake’s “Bathtub Lecture” here in Sils-Maria at the European Club for Fetal Surgery in 2017, may one day provide a life-saving bridge to take premature babies safely from 23–24 weeks’ gestation with normal growth and development to 28–30 weeks’ gestation. Fetal gene therapy and in utero gene editing using CRISPR technology to treat single gene disorders now has proof of principle in fetal animal models.
Fetal Surgery Yet to Come: The Artificial Womb, Big Data, Cells, and Genes
Looking to the future, I shed my cloak, a symbolic rebirth (Fig. 5). We tend to overestimate what will happen in the next year or two, and underestimate what will be accomplished 20 years from now.
There is much more to be done, which requires research – the basis for Fetal Surgery Yet to Come. One of my teachers at Harvard Medical School and Boston Children’s Hospital, Dr. Judah Folkman, taught me that:
As long as there is an unconquered disease, an injury that cannot be repaired, or a method of prevention that remains beyond reach, we have an obligation to conduct research. Research represents HOPE, and for many patients and families, hope is the best thing we have to offer. We pursue our investigations so that one day we can offer more than HOPE, we can offer health.
As predicted in the momentous “Bathtub Lecture,” the clinical application of the artificial womb to babies born too soon at 23–24 weeks’ gestation permits continued normal growth and development for 4–5 weeks or more with dramatically better outcomes. This transformative technology in the Neonatal Intensive Care Unit of the future supporting extremely premature babies is indeed A Brave New World.
Collaboration using BIG DATA through organizations such as NAFTNet – all of us working together – will prove especially powerful to provide real-time prognostic information about birth defect outcomes, and to target the unsolved problems to overcome.
I can imagine a future state in which a mother carrying a fetus with spina bifida, diagnosed at 16 weeks’ gestation, will have the spina bifida sealed and protected before birth by injection of specific tissue-engineered components either through a fetoscope or with an ultrasound-guided amniocentesis needle, and avoid the possible complications of the big fetal surgery operations that we do now. Nature-derived tissue-engineered solutions including underwater biological glues, nanotextured biodegradable elastomers, and cell sheet technology, together with the appropriate dollop of mesenchymal stem cells or derived factors to stimulate nerve regeneration, result in enhanced motor and sensory function after fetal spina bifida repair.
Tissue-engineered solutions are crafted involving harvesting multipotent mesenchymal stem cells by amniocentesis, and then – using CDH for example – seeding muscle progenitor cells onto an acellular matrix to “grow” diaphragm for autologous diaphragmatic reconstruction after birth.
Solving the problem of membrane disruption at fetoscopic port sites permits complex minimally invasive fetal surgery procedures including the use of robotic technology.
Prenatal neuroprotection strategies improve neurodevelopmental outcomes by protecting the brain before birth – for example, in babies with complex congenital heart disease.
Whole-exome and whole-genome sequencing of the triad (mother, father, fetus) for specific birth defects sheds light on the genetic causes of those defects, and suggests therapeutic strategies for prenatal treatment.
Advances in prenatal diagnosis allows the prenatal treatment of anticipated postnatal diseases. Fetal gene therapy and in utero gene editing using prime editing with CRISPR technology are ethically applied clinically to single gene disorders and provide cures for thousands and thousands of unborn patients. A better understanding of maternal-fetal immunology makes in utero hematopoietic stem cell transplantation successful to treat cellular deficiency diseases such as sickle cell anemia, as well as other hematologic and immunologic disorders. Delineation of the immunologic “cross-talk” within the maternal-placental-fetal unit enhances our understanding and treatment of autoimmune diseases and preterm labor.
So… Fetal Surgery Yet To Come: I believe that the future is DAZZLINGLY BRIGHT (Fig. 6)!

Fig. 6: Fetal Surgery Yet to Come. Dr. Adzick holding the IFMSS Tower Lecture Award, consisting of a Julier Tower model embedded on a piece of rock from the famous Julier Pass in the Swiss Alps. He is surrounded by former pediatric and fetal surgeons who he has trained and who represent the future of the field.
Disclosure Statement
The author has no conflicts of interest to declare.
Author Contributions
Dr. N. Scott Adzick is the sole contributor to this article.
Contact us
Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment