The diagnosis and treatment of eosinophilic esophagitis is often very challenging, requiring management from multiple subspecialties. CHOP’s Center for Pediatric Eosinophilic Disorders integrates care from Gastroenterology, Allergy, and Nutrition to create a program that provides personalized care for children with eosinophilic disorders like eosinophilic esophagitis.
Diagnosis
Eosinophilic esophagitis patients present with symptoms that vary by age and can mimic other disorders. Infants and toddlers present with reflux, vomiting, refusal to eat, poor weight gain, and failure to thrive. Older children and adolescents may have these symptoms or more specific esophageal symptoms such as dysphagia or mealtime behaviors that make eating more comfortable. These include: chewing and eating slowly, drinking copious liquids at meals, and avoiding dry or difficult-to-chew foods.
Although gross changes like furrowing or white plaques can be seen at the time of endoscopic evaluation, the esophagus can appear normal despite the presence of clinically significant inflammation. Esophageal biopsies demonstrating mucosal infiltration of over 15 eosinophils per high-powered microscopy field are the gold standard for the diagnosis of eosinophilic esophagitis. Eosinophilic esophagitis is not an immunoglobulin E-mediated food allergy, and skin and serum food testing are not sensitive predictors of if a patient will develop esophageal inflammation to the major food allergens in eosinophilic esophagitis. Therefore, when changes in therapy are made, upper endoscopy with esophageal biopsy is the only option to assess if the therapy is effective at eliminating esophageal inflammation.
Research Horizons: Cutting-edge Techniques to Monitor Disease
EndoFLIP: Over time, the esophageal inflammation that occurs in eosinophilic esophagitis leads to stiffening and narrowing of the esophagus. To date, there is no effective way to objectively characterize and predict changes in esophageal diameter or stiffness. The EndoFLIP® (Endolumenal Functional Lumenal Imaging Probe; Medtronic) imaging system is a technology developed to measure the dimensions and function of a variety of hollow organs, including the esophagus.
With this device we can measure esophageal diameter and pressure in real time by inflating a balloon within the esophagus. We have performed these measurements on more than 400 children at CHOP. We have found that children with eosinophilic esophagitis have decreased esophageal distensibility compared to healthy control patients. In the future, we hope that this tool will serve as the standard of care for monitoring stiffness in eosinophilic esophagitis. Early detection of esophageal stiffness will lead to more aggressive therapy early in the course of disease and could significantly decrease the long-term complications through early intervention.
Transnasal endoscopy: In pediatrics, there is often discordance between symptoms and biopsy results, making endoscopy with anesthesia a frequent occurrence for patients with eosinophilic esophagitis. Understanding disease activity without requiring anesthesia has not been possible until recently. We can now utilize transnasal endoscopies as an alternative for some older children. These scopes are performed through the nasal passage while children watch their favorite shows on TV. We are able to take painless biopsies in 5 to 7 minutes, thus providing an anesthesia-free alternative for older children.
Treatment
Eosinophilic esophagitis can be managed by either pharmacologic therapy or dietary avoidance of food allergens. High-dose proton pump inhibitors (1-2 mg/kg/day) are effective at reducing esophageal inflammation to some degree in approximately 30% to 50% of patients. Swallowed topical budesonide or fluticasone propionate are effective in up to 60% to 70% of patients.
The two most common food allergens responsible for eosinophilic esophagitis in the pediatric population are milk and wheat, however numerous allergens have been implicated in this disorder, highlighting the need for a careful dietary history.
Unfortunately, there are no noninvasive tests which can predict which treatments would be appropriate for a particular patient, and therefore patients undergo repeat endoscopies to evaluate treatment response.
Research Horizons: Potential Diagnostic Testing
We have collaborated with the Gastrointestinal Epithelial Modeling Program (GEM) to develop an esophageal epithelial organoid platform, in which we can model the esophageal microanatomy in a test tube. We can then mimic the inflammatory milieu of eosinophilic esophagitis and screen drugs that may ameliorate this inflammation.
Additional research efforts in CHOP’s Food Allergy Center Frontier Program is focused on understanding how the immune system responds to allergen in eosinophilic esophagitis patients. In the future, we hope that these research efforts will lead to assays that help tailor therapy for eosinophilic esophagitis patients and shorten the time required to find an effective therapeutic regimen.
Our multidisciplinary team at the CHOP Center for Pediatric Eosinophilic Disorders is dedicated to excellence in the care of patients with eosinophilic esophagitis. We are committed to improving the quality of life for our patients, and this drives our research mission, which is focused on improving diagnosis and treatment. In addition to caring for children with eosinophilic esophagitis, we have expertise in caring for other eosinophilic disorders, such as eosinophilic gastroenteritis and hypereosinophilic syndromes.
Figure 1: Endoscopy vs. FLIP study
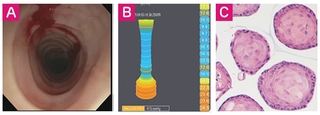
A. Endoscopic view depicting esophagus in the setting of EoE. Patient demonstrates concentric rings and luminal narrowing. The endoscopy caused a tear within the esophageal mucosa due to fibrosis. B. FLIP study showing decreased esophageal distensibility of the esophagus. C. Primary esophageal epithelial organoid and fibroblast culture derived from patient with EoE. Together, these represent a translational platform to evaluate esophageal function and perform personalized therapeutics and diagnostics.
Featured in this article
Specialties & Programs
The diagnosis and treatment of eosinophilic esophagitis is often very challenging, requiring management from multiple subspecialties. CHOP’s Center for Pediatric Eosinophilic Disorders integrates care from Gastroenterology, Allergy, and Nutrition to create a program that provides personalized care for children with eosinophilic disorders like eosinophilic esophagitis.
Diagnosis
Eosinophilic esophagitis patients present with symptoms that vary by age and can mimic other disorders. Infants and toddlers present with reflux, vomiting, refusal to eat, poor weight gain, and failure to thrive. Older children and adolescents may have these symptoms or more specific esophageal symptoms such as dysphagia or mealtime behaviors that make eating more comfortable. These include: chewing and eating slowly, drinking copious liquids at meals, and avoiding dry or difficult-to-chew foods.
Although gross changes like furrowing or white plaques can be seen at the time of endoscopic evaluation, the esophagus can appear normal despite the presence of clinically significant inflammation. Esophageal biopsies demonstrating mucosal infiltration of over 15 eosinophils per high-powered microscopy field are the gold standard for the diagnosis of eosinophilic esophagitis. Eosinophilic esophagitis is not an immunoglobulin E-mediated food allergy, and skin and serum food testing are not sensitive predictors of if a patient will develop esophageal inflammation to the major food allergens in eosinophilic esophagitis. Therefore, when changes in therapy are made, upper endoscopy with esophageal biopsy is the only option to assess if the therapy is effective at eliminating esophageal inflammation.
Research Horizons: Cutting-edge Techniques to Monitor Disease
EndoFLIP: Over time, the esophageal inflammation that occurs in eosinophilic esophagitis leads to stiffening and narrowing of the esophagus. To date, there is no effective way to objectively characterize and predict changes in esophageal diameter or stiffness. The EndoFLIP® (Endolumenal Functional Lumenal Imaging Probe; Medtronic) imaging system is a technology developed to measure the dimensions and function of a variety of hollow organs, including the esophagus.
With this device we can measure esophageal diameter and pressure in real time by inflating a balloon within the esophagus. We have performed these measurements on more than 400 children at CHOP. We have found that children with eosinophilic esophagitis have decreased esophageal distensibility compared to healthy control patients. In the future, we hope that this tool will serve as the standard of care for monitoring stiffness in eosinophilic esophagitis. Early detection of esophageal stiffness will lead to more aggressive therapy early in the course of disease and could significantly decrease the long-term complications through early intervention.
Transnasal endoscopy: In pediatrics, there is often discordance between symptoms and biopsy results, making endoscopy with anesthesia a frequent occurrence for patients with eosinophilic esophagitis. Understanding disease activity without requiring anesthesia has not been possible until recently. We can now utilize transnasal endoscopies as an alternative for some older children. These scopes are performed through the nasal passage while children watch their favorite shows on TV. We are able to take painless biopsies in 5 to 7 minutes, thus providing an anesthesia-free alternative for older children.
Treatment
Eosinophilic esophagitis can be managed by either pharmacologic therapy or dietary avoidance of food allergens. High-dose proton pump inhibitors (1-2 mg/kg/day) are effective at reducing esophageal inflammation to some degree in approximately 30% to 50% of patients. Swallowed topical budesonide or fluticasone propionate are effective in up to 60% to 70% of patients.
The two most common food allergens responsible for eosinophilic esophagitis in the pediatric population are milk and wheat, however numerous allergens have been implicated in this disorder, highlighting the need for a careful dietary history.
Unfortunately, there are no noninvasive tests which can predict which treatments would be appropriate for a particular patient, and therefore patients undergo repeat endoscopies to evaluate treatment response.
Research Horizons: Potential Diagnostic Testing
We have collaborated with the Gastrointestinal Epithelial Modeling Program (GEM) to develop an esophageal epithelial organoid platform, in which we can model the esophageal microanatomy in a test tube. We can then mimic the inflammatory milieu of eosinophilic esophagitis and screen drugs that may ameliorate this inflammation.
Additional research efforts in CHOP’s Food Allergy Center Frontier Program is focused on understanding how the immune system responds to allergen in eosinophilic esophagitis patients. In the future, we hope that these research efforts will lead to assays that help tailor therapy for eosinophilic esophagitis patients and shorten the time required to find an effective therapeutic regimen.
Our multidisciplinary team at the CHOP Center for Pediatric Eosinophilic Disorders is dedicated to excellence in the care of patients with eosinophilic esophagitis. We are committed to improving the quality of life for our patients, and this drives our research mission, which is focused on improving diagnosis and treatment. In addition to caring for children with eosinophilic esophagitis, we have expertise in caring for other eosinophilic disorders, such as eosinophilic gastroenteritis and hypereosinophilic syndromes.
Figure 1: Endoscopy vs. FLIP study
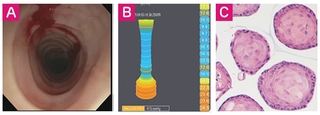
A. Endoscopic view depicting esophagus in the setting of EoE. Patient demonstrates concentric rings and luminal narrowing. The endoscopy caused a tear within the esophageal mucosa due to fibrosis. B. FLIP study showing decreased esophageal distensibility of the esophagus. C. Primary esophageal epithelial organoid and fibroblast culture derived from patient with EoE. Together, these represent a translational platform to evaluate esophageal function and perform personalized therapeutics and diagnostics.
Contact us
Center for Pediatric Eosinophilic Disorders