
An interprofessional team at Children’s Hospital of Philadelphia is transforming CHOP’s approach to fetal medicine through a first-of-its-kind data integration platform. The Clinical Outcomes Data Archive (CODA) platform offers clinicians real-time data to help inform earlier interventions and treatment strategies in CHOP’s Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment (CFDT). A paper outlining CODA’s benefits, applications and potential broader impact was recently published in the journal Fetal Diagnosis and Therapy.
In today’s health systems, Electronic Heath Records (EHRs) are typically the standard for efficient data collection of common elements of patient interaction with healthcare systems. However, EHRs pose significant limitations because the most important elements of diagnosis and care for patients are not easily extractable from the EHR. Further, in the context of prenatal diagnosis and treatment, the fetus lacks its own digital identity requiring complex relinking of fetal attributes documented in the maternal chart to data from their pediatric record once born. This challenge is amplified when multiple gestations, returning maternal patients and pregnancy loss are factored in.
The late Lori J. Howell, DNP, MS, RN, former CFDT Executive Director, long-held a goal for CHOP to offer meaningful, real-time, risk adjusted outcomes information for fetal patients and their families. To achieve this vision, a new approach to data management was designed by Matthew Goldshore, MD, PhD, MPH, a pediatric surgery fellow with CHOP’s Division of Pediatric General, Thoracic and Fetal Surgery, and CFDT Business Manager Tom Reynolds, MFA, MBA. The technology powering CODA was developed by an interprofessional team led by Reynolds, and workflows which integrate EHR data with manually collected and clinically reviewed information were set in motion. Within this framework, the CODA team created a large-scale “living” analytic-grade database, which now supports real-time clinical outcomes reporting across the CFDT.
“One of our key challenges in fetal care has been in effectively analyzing data from the EHR, particularly for patients with congenital abnormalities,” said Holly Hedrick, MD, Primary Investigator and lead clinical sponsor and an attending pediatric and fetal surgeon in the Division of Pediatric General, Thoracic and Fetal Surgery at CHOP. “Traditional EHR systems are not well-equipped to capture the nuances of fetal health, which evolve over time and across different medical specialties. CODA’s success in merging EHR-sourced and manually abstracted data will transform how healthcare providers manage and study pregnancy-related outcomes.”
CODA has curated data for each mother and fetus born in CHOP’s Garbose Family Special Delivery Unit since 2013 from prenatal diagnosis, perinatal care and delivery and continues to document their treatment and outcomes during their life-long interaction with CHOP. In the recently published paper, the researchers noted that CODA offers substantial benefits to clinicians, surpassing the capabilities of studies relying on data extracted from the EHR alone. For example, 85% of condition-specific variables required manual abstraction, highlighting the need for careful review of narrative documentation of ongoing follow-up in studying patients with birth defects, as many outcomes emerge later in childhood, influenced by complex, multi-level factors (e.g., individual, family, policy).
As of today, CODA has validated more than 15 million data points from more than 15,000 patients across dozens of conditions. In addition to supporting enhanced patient care, CODA expedites clinical and translational research, significantly reducing the time required to answer pressing questions with high-quality data. By contributing their unique experiences, each patient plays a critical role in advancing the understanding of rare conditions. In fact, CODA’s ability to unify complex data across multiple stages of maternal and pediatric care has already contributed to more than 70 research initiatives and offers a path forward for more reliable, ongoing research in maternal-fetal health.
Moving forward, the team is enhancing automation of manual EHR abstraction by improving the design of documentation in the EHR and employing general large language models to automate data capture within the CODA framework. They are also integrating multimodal data sources, including physiologic data from monitors and high-frequency data from comprehensive diagnostic studies, with the clinical data in CODA to enrich research and improve prognostication.
“By applying what we learn to pave the way forward, we can create better lives for our patients and their families,” said Hedrick.
The development of CODA and ongoing research was funded by the philanthropy of families of the CFDT and internal funding through the CHOP Frontier Programs and CHOP Information Services.
Reynolds et al, “A Clinical Outcomes Data Archive for a Comprehensive Fetal Diagnosis and Treatment Center.” Fetal Diagn Ther. Online October 8, 2024. DOI: 10.1159/000541877.
Featured in this article
Experts
Specialties & Programs
An interprofessional team at Children’s Hospital of Philadelphia is transforming CHOP’s approach to fetal medicine through a first-of-its-kind data integration platform. The Clinical Outcomes Data Archive (CODA) platform offers clinicians real-time data to help inform earlier interventions and treatment strategies in CHOP’s Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment (CFDT). A paper outlining CODA’s benefits, applications and potential broader impact was recently published in the journal Fetal Diagnosis and Therapy.
In today’s health systems, Electronic Heath Records (EHRs) are typically the standard for efficient data collection of common elements of patient interaction with healthcare systems. However, EHRs pose significant limitations because the most important elements of diagnosis and care for patients are not easily extractable from the EHR. Further, in the context of prenatal diagnosis and treatment, the fetus lacks its own digital identity requiring complex relinking of fetal attributes documented in the maternal chart to data from their pediatric record once born. This challenge is amplified when multiple gestations, returning maternal patients and pregnancy loss are factored in.
The late Lori J. Howell, DNP, MS, RN, former CFDT Executive Director, long-held a goal for CHOP to offer meaningful, real-time, risk adjusted outcomes information for fetal patients and their families. To achieve this vision, a new approach to data management was designed by Matthew Goldshore, MD, PhD, MPH, a pediatric surgery fellow with CHOP’s Division of Pediatric General, Thoracic and Fetal Surgery, and CFDT Business Manager Tom Reynolds, MFA, MBA. The technology powering CODA was developed by an interprofessional team led by Reynolds, and workflows which integrate EHR data with manually collected and clinically reviewed information were set in motion. Within this framework, the CODA team created a large-scale “living” analytic-grade database, which now supports real-time clinical outcomes reporting across the CFDT.
“One of our key challenges in fetal care has been in effectively analyzing data from the EHR, particularly for patients with congenital abnormalities,” said Holly Hedrick, MD, Primary Investigator and lead clinical sponsor and an attending pediatric and fetal surgeon in the Division of Pediatric General, Thoracic and Fetal Surgery at CHOP. “Traditional EHR systems are not well-equipped to capture the nuances of fetal health, which evolve over time and across different medical specialties. CODA’s success in merging EHR-sourced and manually abstracted data will transform how healthcare providers manage and study pregnancy-related outcomes.”
CODA has curated data for each mother and fetus born in CHOP’s Garbose Family Special Delivery Unit since 2013 from prenatal diagnosis, perinatal care and delivery and continues to document their treatment and outcomes during their life-long interaction with CHOP. In the recently published paper, the researchers noted that CODA offers substantial benefits to clinicians, surpassing the capabilities of studies relying on data extracted from the EHR alone. For example, 85% of condition-specific variables required manual abstraction, highlighting the need for careful review of narrative documentation of ongoing follow-up in studying patients with birth defects, as many outcomes emerge later in childhood, influenced by complex, multi-level factors (e.g., individual, family, policy).
As of today, CODA has validated more than 15 million data points from more than 15,000 patients across dozens of conditions. In addition to supporting enhanced patient care, CODA expedites clinical and translational research, significantly reducing the time required to answer pressing questions with high-quality data. By contributing their unique experiences, each patient plays a critical role in advancing the understanding of rare conditions. In fact, CODA’s ability to unify complex data across multiple stages of maternal and pediatric care has already contributed to more than 70 research initiatives and offers a path forward for more reliable, ongoing research in maternal-fetal health.
Moving forward, the team is enhancing automation of manual EHR abstraction by improving the design of documentation in the EHR and employing general large language models to automate data capture within the CODA framework. They are also integrating multimodal data sources, including physiologic data from monitors and high-frequency data from comprehensive diagnostic studies, with the clinical data in CODA to enrich research and improve prognostication.
“By applying what we learn to pave the way forward, we can create better lives for our patients and their families,” said Hedrick.
The development of CODA and ongoing research was funded by the philanthropy of families of the CFDT and internal funding through the CHOP Frontier Programs and CHOP Information Services.
Reynolds et al, “A Clinical Outcomes Data Archive for a Comprehensive Fetal Diagnosis and Treatment Center.” Fetal Diagn Ther. Online October 8, 2024. DOI: 10.1159/000541877.
Recommended reading
A Lifesaving Fetal Heart Surgery
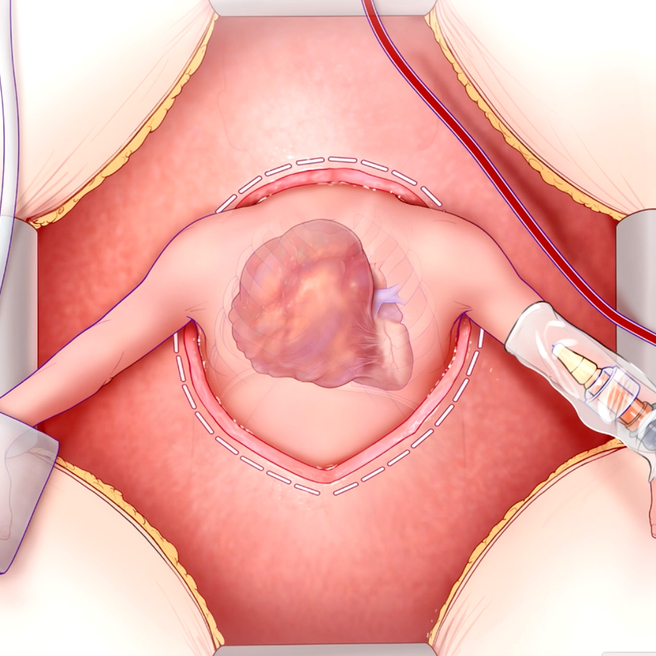
CHOP’s Center for Fetal Diagnosis and Treatment and Fetal Heart Program, successfully remove rare tumor from baby’s heart while still in the womb.
Contact us
Ashley Moore
Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment