It’s not just you; everyone hates their electronic health record (EHR). When surveyed about causes of burnout, the EHR is always one of the top things healthcare providers point to. There are multiple reasons for this, all which stretch providers thinner and thinner. Firstly, studies have shown that providers spend up to two-thirds of their clinic time on EHR and clerical tasks and only a third on medical care. Secondly, the documentation burden in the United States (compared to internationally) is enormous, and providers must add more stuff and click more buttons to keep up with the regulations. Both of these factors lead to less face-to-face time with patients, more time finishing notes after clinic, and more “pajama time” taken up by the EHR.
Additionally, EHRs are extraordinarily complex pieces of software which are difficult to learn. When you first go live, often with reduced clinical schedules and many support staff to aid in the transition, you have time to open yourself up to learn new workflows. But, when the trainers leave and the schedules go back to normal, and you have embraced that initial way of doing things that you first learned. Most providers feel a sense of isolation—the trainers aren’t coming back and you get little-to-no information on upgrades or new functionality. Although, even if you did, it’s difficult to incorporate the new stuff into the workflows you first imprinted on, even if they may make you more efficient!
The good news is that there are a number of efforts across the country to improve EHR-related burnout: The 21st Century Cures legislation is pushing for streamlined documentation; EHR vendors are actively working to improve the usability of their software and improve provider efficiency tools; many healthcare organizations are starting “optimization” programs designed to improve efficiency like Stanford’s “Home4Dinner” and Riley Children’s “Pajama Time,” where providers get targeted retraining and help building their own personalized tools.
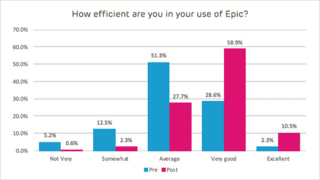
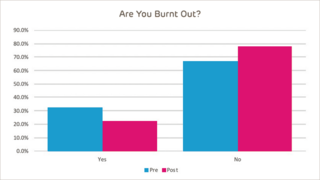
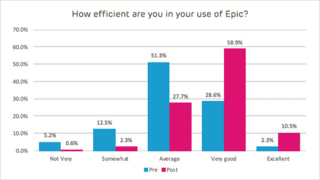
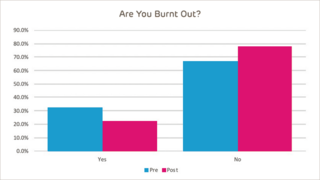
At Children’s Hospital of Philadelphia (CHOP), we have spent the last 3 years on our own optimization program called “HeathyEHR Users.” Our focus was on retraining, and we gave every provider in our organization at least 1 hour of one-on-one time with an EHR trainer outside of patient care to customize their EHR workspaces and to learn (or relearn) many of the basic tools needed to be efficient. Our providers found these sessions very helpful, reporting a 21% improvement in how efficient they felt. They even reported a 32% decrease in burnout, showing that it is possible to feel better about both your EHR and your job.
Even if you are not part of an organization that can provide such programs, there are still things you can do to improve your efficiency:
- Customize your experience – Most vendors build in the ability for users to customize their workspace. Spending a little time to set up your EMR how you like it can make an enormous difference in your efficiency. Some ways you might be able to customize are:
- Common orders with your own personal defaults
- Common diagnoses, chief complaints, or reason for follow-up
- Documentation templates or phrases
It is important that you give yourself time outside of patient care to do this; trying to learn EHR stuff during a busy clinic day is a recipe for disaster!
- Re-training – EHR vendors are often updating their software to be easier and more efficient to use. However, it is very difficult for busy clinicians to both hear about these changes (they usually come in an email or tip sheet, if they come at all) and incorporate them into their workflows. Reach out to your vendor and see if it can send a trainer or analyst to your site to do some teaching. Whether it’s one-on-one, at-the-elbow, or a lunch and learn, having an expert show you some efficiency-gaining tips, as well as hearing your particular needs, can be quite valuable.
- Reduce the burden of documentation – Removing excessive typing from your workflow can make a world of difference! Many providers are using voice-to-text products to do partial dictation in their notes (eg, dictate your HPI, assessment, and plan and use existing templates for ROS and physical exam), thus reducing the amount of keyboard time necessary in an office visit. Also, scribes are becoming more and more prevalent in healthcare. Although is this a more expensive options, they have been shown to be greatly improve efficiency while reducing documentation burden. Consider exploring a cost/benefit analysis of these options.
- Don’t be isolated – Where you may be struggling with your EHR, a colleague may be doing much better. Whether it be in your own clinic, regionally, or nationally, seek out others that use your EHR to share successes, struggles, and efficiency tips.
Yes, burnout is an important issue in healthcare and, yes, the EHR is a major factor in its rise. However, you can combat it in your clinic or organization. Take the time to improve your efficiency and you may also find yourself feeling better about your interactions with your EHR, and possibly more.
It’s not just you; everyone hates their electronic health record (EHR). When surveyed about causes of burnout, the EHR is always one of the top things healthcare providers point to. There are multiple reasons for this, all which stretch providers thinner and thinner. Firstly, studies have shown that providers spend up to two-thirds of their clinic time on EHR and clerical tasks and only a third on medical care. Secondly, the documentation burden in the United States (compared to internationally) is enormous, and providers must add more stuff and click more buttons to keep up with the regulations. Both of these factors lead to less face-to-face time with patients, more time finishing notes after clinic, and more “pajama time” taken up by the EHR.
Additionally, EHRs are extraordinarily complex pieces of software which are difficult to learn. When you first go live, often with reduced clinical schedules and many support staff to aid in the transition, you have time to open yourself up to learn new workflows. But, when the trainers leave and the schedules go back to normal, and you have embraced that initial way of doing things that you first learned. Most providers feel a sense of isolation—the trainers aren’t coming back and you get little-to-no information on upgrades or new functionality. Although, even if you did, it’s difficult to incorporate the new stuff into the workflows you first imprinted on, even if they may make you more efficient!
The good news is that there are a number of efforts across the country to improve EHR-related burnout: The 21st Century Cures legislation is pushing for streamlined documentation; EHR vendors are actively working to improve the usability of their software and improve provider efficiency tools; many healthcare organizations are starting “optimization” programs designed to improve efficiency like Stanford’s “Home4Dinner” and Riley Children’s “Pajama Time,” where providers get targeted retraining and help building their own personalized tools.
At Children’s Hospital of Philadelphia (CHOP), we have spent the last 3 years on our own optimization program called “HeathyEHR Users.” Our focus was on retraining, and we gave every provider in our organization at least 1 hour of one-on-one time with an EHR trainer outside of patient care to customize their EHR workspaces and to learn (or relearn) many of the basic tools needed to be efficient. Our providers found these sessions very helpful, reporting a 21% improvement in how efficient they felt. They even reported a 32% decrease in burnout, showing that it is possible to feel better about both your EHR and your job.
Even if you are not part of an organization that can provide such programs, there are still things you can do to improve your efficiency:
- Customize your experience – Most vendors build in the ability for users to customize their workspace. Spending a little time to set up your EMR how you like it can make an enormous difference in your efficiency. Some ways you might be able to customize are:
- Common orders with your own personal defaults
- Common diagnoses, chief complaints, or reason for follow-up
- Documentation templates or phrases
It is important that you give yourself time outside of patient care to do this; trying to learn EHR stuff during a busy clinic day is a recipe for disaster!
- Re-training – EHR vendors are often updating their software to be easier and more efficient to use. However, it is very difficult for busy clinicians to both hear about these changes (they usually come in an email or tip sheet, if they come at all) and incorporate them into their workflows. Reach out to your vendor and see if it can send a trainer or analyst to your site to do some teaching. Whether it’s one-on-one, at-the-elbow, or a lunch and learn, having an expert show you some efficiency-gaining tips, as well as hearing your particular needs, can be quite valuable.
- Reduce the burden of documentation – Removing excessive typing from your workflow can make a world of difference! Many providers are using voice-to-text products to do partial dictation in their notes (eg, dictate your HPI, assessment, and plan and use existing templates for ROS and physical exam), thus reducing the amount of keyboard time necessary in an office visit. Also, scribes are becoming more and more prevalent in healthcare. Although is this a more expensive options, they have been shown to be greatly improve efficiency while reducing documentation burden. Consider exploring a cost/benefit analysis of these options.
- Don’t be isolated – Where you may be struggling with your EHR, a colleague may be doing much better. Whether it be in your own clinic, regionally, or nationally, seek out others that use your EHR to share successes, struggles, and efficiency tips.
Yes, burnout is an important issue in healthcare and, yes, the EHR is a major factor in its rise. However, you can combat it in your clinic or organization. Take the time to improve your efficiency and you may also find yourself feeling better about your interactions with your EHR, and possibly more.