Ryan C. Borek, MD; Ashley Williams, CRNP
Case: L.C., a 14-year-old male, was referred to our clinic for evaluation of obstructive sleep apnea. He has a history of trisomy 21 and underwent a tonsillectomy and adenoidectomy (T&A) at age 3. He continued to show signs of persistent apnea, including restless sleep, daytime tiredness, snoring with audible pauses, and behavior changes. At age 10 he underwent an overnight sleep study documenting an obstructive AHI (apnea-hypopnea index) of 27 events/hour (severe) with associated desaturations. He was started on CPAP (continuous positive airway pressure) and tolerated it for a few years. At age 12 a repeat sleep study was performed because he was no longer tolerating CPAP and showing signs of worsening apnea. Results of the repeat sleep study indicated severe OSA with an obstructive AHI of 32.2 events/hour and a nadir oxygen saturation of 80%.
Initial clinical evaluation showed absent tonsils and BMI of 19 kg/m2 (56% for age). We discussed options, and the family elected to perform a drug- induced sleep endoscopy (DISE), which is an evaluation of airway dynamics with anesthetic induced “sleep.” This examination showed absent adenoids and tonsils but noted multi-level collapse of the soft palate and base of tongue. Given these findings, we discussed hypoglossal nerve stimulator (HGN) implantation as an alternative sleep apnea treatment. L.C. recently underwent successful surgical implantation and recovered well. On follow-up discussion with family members, they report he is doing well and sleeping through the night!
Discussion: Persistent sleep apnea after T&A is a frequent problem encountered in pediatrics and is more common in patients with obesity, neuromuscular disorders, and craniofacial syndromes, including Down syndrome. We know that untreated obstructive sleep apnea can lead to cardiac, metabolic, and behavioral sequela. CPAP is an excellent non- surgical treatment, but adherence to treatment is difficult to maintain. Our advanced sleep program at CHOP is designed to assess surgical options for treatment of persistent OSA after T&A. We encompass a multidisciplinary approach with the hospital’s Pulmonary, Plastic Surgery, and Oral and Maxillofacial Surgery programs to offer treatment options past CPAP if possible.
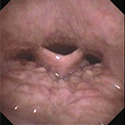
Our evaluation starts with a clinical history, physical examination, and review of the most recent sleep study. In patients with OSA, if the cause of obstruction is unidentified, we offer DISE to evaluate possible sites of obstruction. DISE is a procedure in the operating room where a flexible scope is passed into the nose to evaluate the upper airway during pharmacologic “sleep” induced by anesthesia. This procedure identifies sites of obstruction. Possible sites of obstruction can originate at any point in the airway from the nasal cavity to the lower airway. Table 1 identifies sites of obstruction and possible surgical options. Figure 1 image from a DISE demonstrates tongue base obstruction causing airway narrowing.
Table 1: Sites of Obstruction
Obstructive Sites
- nasal turbinate hypertrophy
- nasal septal deviation
- adenoid hypertrophy
- soft palate (velum) obstruction
- tonsillar hypertrophy
- maxillary/mandibular hypoplasia
- lingual hypertrophy
- laryngomalacia
- subglottic stenosis
- tracheal tenosis
Surgical Options
- turbinate reduction
- septoplasty
- adenoidectomy
- pharyngoplasty
- Tonsillectomy
- maxillomandibular advancement
- lingual tonsillectomy
- supraglottoplasty, partial epiglottectomy
- laryngotracheal reconstruction
- tracheoplasty
Hypoglossal nerve stimulator: recent approval for ages 13 – 18
HGN stimulation is an exciting alternative therapy for certain pediatric patients with obstructive sleep apnea. This system uses an implantable device to stimulate the hypoglossal nerve to protrude the tongue during respiration. This device has been shown to be safe and effective in adolescents with Down syndrome, and has been recently approved by the Food and Drug Administration for patients ages 13 to 18 years with severe OSA. The implant therapy is activated via remote control each night when the patient goes to sleep and turned off upon awakening.

During the surgery, 2 incisions are made and the implant is tunneled under the skin to connect the nerve stimulator and the respiratory sensing lead (see Figure 2). Before implantation, patients must undergo a DISE procedure to ensure the patient is a candidate for hypoglossal nerve stimulation.
Our advanced sleep providers are look forward to working with patients and families with persistent sleep apnea.
References and suggested readings
Diercks GR, Wentland C, Keamy D, et al. Hypoglossal nerve stimulation in adolescents with Down syndrome and obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg. 2018;144(1):37-42.
Bluher AE, Ishman SL, Baldassari CM. Managing the child with persistent sleep apnea. Otolaryngol Clin North Am. 2019;52(5):891-901.
Ryan C. Borek, MD; Ashley Williams, CRNP
Case: L.C., a 14-year-old male, was referred to our clinic for evaluation of obstructive sleep apnea. He has a history of trisomy 21 and underwent a tonsillectomy and adenoidectomy (T&A) at age 3. He continued to show signs of persistent apnea, including restless sleep, daytime tiredness, snoring with audible pauses, and behavior changes. At age 10 he underwent an overnight sleep study documenting an obstructive AHI (apnea-hypopnea index) of 27 events/hour (severe) with associated desaturations. He was started on CPAP (continuous positive airway pressure) and tolerated it for a few years. At age 12 a repeat sleep study was performed because he was no longer tolerating CPAP and showing signs of worsening apnea. Results of the repeat sleep study indicated severe OSA with an obstructive AHI of 32.2 events/hour and a nadir oxygen saturation of 80%.
Initial clinical evaluation showed absent tonsils and BMI of 19 kg/m2 (56% for age). We discussed options, and the family elected to perform a drug- induced sleep endoscopy (DISE), which is an evaluation of airway dynamics with anesthetic induced “sleep.” This examination showed absent adenoids and tonsils but noted multi-level collapse of the soft palate and base of tongue. Given these findings, we discussed hypoglossal nerve stimulator (HGN) implantation as an alternative sleep apnea treatment. L.C. recently underwent successful surgical implantation and recovered well. On follow-up discussion with family members, they report he is doing well and sleeping through the night!
Discussion: Persistent sleep apnea after T&A is a frequent problem encountered in pediatrics and is more common in patients with obesity, neuromuscular disorders, and craniofacial syndromes, including Down syndrome. We know that untreated obstructive sleep apnea can lead to cardiac, metabolic, and behavioral sequela. CPAP is an excellent non- surgical treatment, but adherence to treatment is difficult to maintain. Our advanced sleep program at CHOP is designed to assess surgical options for treatment of persistent OSA after T&A. We encompass a multidisciplinary approach with the hospital’s Pulmonary, Plastic Surgery, and Oral and Maxillofacial Surgery programs to offer treatment options past CPAP if possible.
Our evaluation starts with a clinical history, physical examination, and review of the most recent sleep study. In patients with OSA, if the cause of obstruction is unidentified, we offer DISE to evaluate possible sites of obstruction. DISE is a procedure in the operating room where a flexible scope is passed into the nose to evaluate the upper airway during pharmacologic “sleep” induced by anesthesia. This procedure identifies sites of obstruction. Possible sites of obstruction can originate at any point in the airway from the nasal cavity to the lower airway. Table 1 identifies sites of obstruction and possible surgical options. Figure 1 image from a DISE demonstrates tongue base obstruction causing airway narrowing.
Table 1: Sites of Obstruction
Obstructive Sites
- nasal turbinate hypertrophy
- nasal septal deviation
- adenoid hypertrophy
- soft palate (velum) obstruction
- tonsillar hypertrophy
- maxillary/mandibular hypoplasia
- lingual hypertrophy
- laryngomalacia
- subglottic stenosis
- tracheal tenosis
Surgical Options
- turbinate reduction
- septoplasty
- adenoidectomy
- pharyngoplasty
- Tonsillectomy
- maxillomandibular advancement
- lingual tonsillectomy
- supraglottoplasty, partial epiglottectomy
- laryngotracheal reconstruction
- tracheoplasty
Hypoglossal nerve stimulator: recent approval for ages 13 – 18
HGN stimulation is an exciting alternative therapy for certain pediatric patients with obstructive sleep apnea. This system uses an implantable device to stimulate the hypoglossal nerve to protrude the tongue during respiration. This device has been shown to be safe and effective in adolescents with Down syndrome, and has been recently approved by the Food and Drug Administration for patients ages 13 to 18 years with severe OSA. The implant therapy is activated via remote control each night when the patient goes to sleep and turned off upon awakening.

During the surgery, 2 incisions are made and the implant is tunneled under the skin to connect the nerve stimulator and the respiratory sensing lead (see Figure 2). Before implantation, patients must undergo a DISE procedure to ensure the patient is a candidate for hypoglossal nerve stimulation.
Our advanced sleep providers are look forward to working with patients and families with persistent sleep apnea.
References and suggested readings
Diercks GR, Wentland C, Keamy D, et al. Hypoglossal nerve stimulation in adolescents with Down syndrome and obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg. 2018;144(1):37-42.
Bluher AE, Ishman SL, Baldassari CM. Managing the child with persistent sleep apnea. Otolaryngol Clin North Am. 2019;52(5):891-901.