Arley’s Story: Fetal Surgery for Pericardial Teratoma
Arley’s Story: Fetal Surgery for Pericardial Teratoma
During an ultrasound at 24 weeks gestation, Brailey and Louis learned a tumor was growing on their unborn daughter Arley’s heart. Suddenly, what had seemed like a routine pregnancy was a life-threatening situation.
They quickly met with a pediatric cardiologist in their home state of Tennessee, and he told them time was running out. The tumor — called a pericardial teratoma — develops inside the sac that surrounds the heart. As the tumor grows, it can compress the heart and prevent the heart from filling and contracting.
The cardiologist said the only hope of saving Arley was fetal surgery to remove the tumor, and the surgery had to be done very soon or the baby would die. He reached out to a colleague known around the world for his experience with pericardial teratoma: Pediatric Cardiologist Jack Rychik, MD, who leads the Fetal Heart Program at Children’s Hospital of Philadelphia (CHOP).
In 2013, a team at CHOP was the first in the world to successfully perform open fetal surgery on the heart to remove a pericardial teratoma. To date, they’ve successfully done the procedure more than any team in the world.
A race against a growing tumor
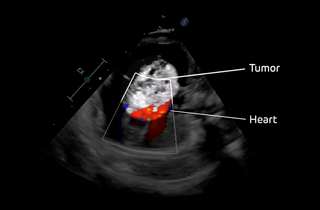
Dr. Rychik reviewed a copy of Brailey’s fetal echocardiogram and saw the potential to make a difference.
“That's when the ball started to roll, and it rolled fast,” says Louis.
The couple flew to Philadelphia for an all-day evaluation. Fetal imaging experts and highly specialized attending radiologists worked with maternal-fetal medicine specialists in CHOP’s Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment to perform and review ultrasound and fetal MRI scans. The Fetal Heart Program team performed a new fetal echocardiogram and used their special expertise to determine when fetal surgery would need to be performed based on the condition of Arley’s heart. Social workers and child life specialists also met with the couple to offer mental, emotional and logistical support.
At the end of the day, the clinical team discussed their findings with the couple. They explained that based on the tumor’s rapid growth, fetal surgery would need to be performed the next day if they wanted any hope of saving their baby.

Brailey and Louis were nervous and scared. In addition to the risks of fetal surgery, after the procedure, Brailey would need to stay in Philadelphia for the rest of the pregnancy for close monitoring in case she went into labor early. Louis had to stay in Tennessee to look after their first child and continue working. It was a lot to take in and take on.
But they decided to go through with the procedure to give Arley the best chance possible. They knew that if anyone could save Arley’s life, it was the team at CHOP.
CHOP’s team knows better than anyone how to minimize the risks of these complex procedures for both mother and baby. They’ve performed more than 2,400 fetal surgeries, more than any other hospital in the world.
Incredible fetal surgery to save Arley’s life
Less than 24 hours after arriving in Philadelphia, Brailey underwent fetal surgery. Arley weighed less than two pounds. She could fit in the palm of your hand.
Performing a procedure as complicated as open fetal surgery on the heart requires experts in cardiology, fetal surgery, maternal-fetal medicine, anesthesiology and neonatology as well as a special cohort of fetal nurses. Teamwork is critical.
An anesthesiologist put Brailey under, placed an epidural catheter for pain control and intubated her. They placed tubes to monitor her blood pressure and provide fluids and medication as needed.
The surgical team — led by Holly Hedrick, MD — included five experts with more than 100 years of combined experience. Fetal surgery is a “well-orchestrated dance” says Dr. Hedrick. Every decision the team makes is informed by decades of experience.
Juliana Sanchez Gebb, MD, the maternal-fetal medicine specialist, used ultrasound to map out the placenta and guide the surgeons on the best place to enter the uterus. Dr. Gebb and the anesthesiologist also monitored Brailey throughout the procedure to ensure she remained stable.

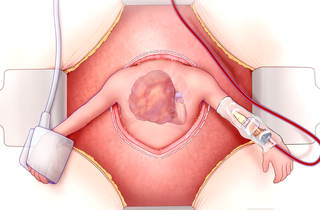
The surgical team made an incision in Brailey’s abdomen and carefully entered the uterus using a special stapling device. Dr. Rychik performed continuous fetal echocardiography to inform the team on how surgery was impacting Arley’s heart and whether blood transfusions or resuscitation were needed.
During fetal surgery, changes in uterine volume can trigger preterm labor. The team uses a special catheter that continuously replaces amniotic fluid in the uterus. They also keep most of the fetus’s body inside the uterus. They only remove the fetus's arms to place an IV for fluids, medications and blood transfusions, and a pulse oximeter to monitor vital signs. The fetus’s chest is then exposed and opened so the tumor can be removed from the heart.
The team’s expertise proved vital when they discovered a small portion of the tumor was connected to Arley’s aorta, which is the body’s main blood vessel. After Pediatric Cardiothoracic Surgeon Katsuhide Maeda, MD, PhD, slowly removed the massive tumor from Arley’s olive-sized heart, there was bleeding from the aorta, which he quickly repaired.
Once the tumor was removed, the team closed Arley’s chest, then they closed the uterus and Brailey’s abdomen. The rest of the pregnancy was followed very closely by a team of many specialists, with weekly ultrasounds to make sure the fetus was developing normally and there were no complications in the uterus. With the tumor gone, Arley’s heart was finally free to expand and contract, and there was no longer the threat of heart failure.
Born with a healthy heart

On Feb. 17, 2024, three months after fetal surgery, Arley was born via c-section in CHOP’s Garbose Family Special Delivery Unit, the world’s first birth facility in a pediatric hospital specifically designed for healthy mothers carrying babies with known birth defects. The delivery unit was created to allow families to stay close by while their babies are treated immediately in CHOP’s intensive care units.
The team delivers the largest number of critically ill infants with birth defects in the nation. After babies are born in the unit, they are immediately carried into a stabilization suite where an expert team is ready and waiting to provide all the support they need. Having this comprehensive care in one location is critically important to the well-being of babies born with complex congenital conditions.
The team placed Arley on a warming bed and assessed her breathing and circulation. They were pleased to see that her heart and lungs were functioning well.
“The first moment I saw her, I remember joy, relief,” says Brailey. “I remember looking to see what her chest might look like. Would there be a significant scar? Would she look different? And she looked perfect.”

Arley recovered in CHOP’s Harriet and Ronald Lassin Newborn/Infant Intensive Care Unit. She spent about three weeks there and then was able to go home to Tennessee. Her parents are beyond thrilled to be able to let her grow up and “do all the normal kid stuff,” says Brailey.
“When I went to medical school, it was unimaginable that we'd be able to perform fetal surgery and get a successful outcome,” says Dr. Rychik. “I have every expectation that Arley will grow into a beautiful, healthy, young girl who will have every opportunity at good health and a good life.”
Arley continues to thrive, joining the three other children who have successfully undergone this fetal surgery procedure at CHOP.
“Each one of these kids and each one of these families are pioneers,” says Dr. Rychik. “There are no individuals who've walked the face of the earth before that have had this condition and have survived except for this handful of individuals who have had fetal surgical resection for this rare pericardial teratoma condition.”