Frequently Asked Questions about Congenital Diaphragmatic Hernia: Helping You Make Choices About Your Child's Care
Published on
Published on
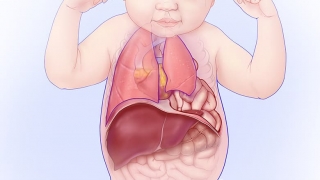 With CDH, a hole in the diaphragm allows abdominal organs to move into the chest. There, they can crowd the heart and lungs and keep the lungs from growing normally. © CHOP/CFDT
Finding out that your unborn baby has congenital diaphragmatic hernia (CDH) can be a scary experience. We know you’ll have many questions about this new diagnosis and what it means for your child and your family.
With CDH, a hole in the diaphragm allows abdominal organs to move into the chest. There, they can crowd the heart and lungs and keep the lungs from growing normally. © CHOP/CFDT
Finding out that your unborn baby has congenital diaphragmatic hernia (CDH) can be a scary experience. We know you’ll have many questions about this new diagnosis and what it means for your child and your family.
Here, we cover many common questions about CDH that our patient families ask our CDH team. Our goal is to provide expecting parents with information that will help them make choices about their child’s care and choose a CDH treatment center that is right for them.
Babies with CDH require immediate care after they’re born. It is important for a baby with CDH to be delivered where they have immediate access to an experienced team that includes neonatologists, pediatric surgeons, advanced practice neonatal surgical nurses, registered nurses, respiratory therapists, nutritionists, cardiologists and pulmonologists, among others. To minimize transport time to the NICU, babies with CDH should be delivered within the same hospital where the NICU is located.
At Children’s Hospital of Philadelphia (CHOP), you will deliver your baby in the same hospital as where your baby will receive care, in our Garbose Family Special Delivery Unit (SDU). Our NICU is just a short distance away from the SDU. You will have 24-hour access to your baby. Parents are a vital part of the baby’s team and we encourage your presence and interaction with your baby as much as possible.
This is an important question to ask any CDH treatment center. Because CDH is such a complex condition and babies require immediate, expert care after birth, it’s important that a hospital has experience caring for the unique needs of these patients.
On average, we care for 50 new CDH patients per year. We currently follow more than 600 CDH patients in our multidisciplinary Pulmonary Hypoplasia Program, which provides long-term follow up and early interventions to optimize our patients’ outcomes.
Most babies born at CHOP with a prenatal diagnosis of CDH do very well. For babies diagnosed with isolated CDH, the location of the liver (above or below the diaphragm) is the best indicator of how well they’ll do after birth. When determining congenital diaphragmatic hernia prognosis, we also take into consideration several measurements that are taken during ultrasound and MRI tests (lung to head ratios and total lung volumes). Other factors impacting their outlook may include the presence of other anomalies or genetic differences.
When a baby with CDH is delivered in CHOP’s SDU, they are immediately handed through a "pass-through" window to the waiting Newborn/Infant Stabilization Team in the adjacent SDU resuscitation room. These rooms are specially designed for the birth of babies who need immediate attention.
A tube is placed into the baby’s airway to help with breathing. Another tube is placed into the baby’s nose or mouth down to the stomach to keep it empty of fluid and air. This gives the baby's lungs more room to expand. Intravenous (IV) lines are placed in the baby’s hands or feet and the umbilical cord to give medications and fluids, as well as to monitor specific blood levels. Once they are stabilized, they are taken to the nearby Newborn/Infant Intensive Care Unit (N/IICU), with dedicated rooms for babies with surgical diagnoses such as CDH.
Gentle ventilation is used on all babies with CDH in our N/IICU. Gentle ventilation refers to providing breathing support to babies with CDH by minimizing the percentage of oxygen, number of breaths, and amount of pressure needed to prevent secondary damage.
ECMO (extracorporeal membrane oxygenation) is a treatment that allows the lungs and heart to rest while a machine takes over their function. We use a specific set of guidelines to indicate if a baby needs to go on ECMO. Learn more about when ECMO is used to treat babies with CDH.
It is important to remember that the heart and lungs need to work together. A pediatric cardiologist specializing in pulmonary hypertension (high blood pressure in the lungs) performs an echocardiogram (echo) shortly after your baby arrives in the N/IICU. The echo is repeated at frequent intervals to assess the baby’s response to medicines that treat pulmonary hypertension. Cardiac catheterization is a treatment option for severe cases.
If your baby has a cardiac difference they may require timely catheterization or surgery. A pulmonologist offers their expertise with medications, readiness to wean from breathing support, innovative breathing interfaces that may avoid tracheostomy and long-term ventilation support.
Stability! It is safer to operate on a stable baby than one who is still critically ill. Stability is determined by degree of pulmonary hypertension, ventilator settings, blood gases, blood pressure, and diuresis.
It can be, but the preference is to wait until the baby is stable enough to not need ECMO.
A patch is used if the hole in the diaphragm is too large to suture (stitch) closed. The patch is placed in such a way that it does not interfere with the baby’s long-term growth.
We encourage breastfeeding and will teach you how to pump your milk. The milk is frozen and stored in our Milk Bank until the baby is ready to start feeds. At that time, the milk will be given by a small tube into the baby’s stomach until the baby is ready to start feeding by mouth.
Feeding can be a challenge for babies with CDH, but our speech therapy team will work closely with you to help you feel comfortable feeding your baby.
You will be able to touch, talk to and hold your baby as soon as it is medically safe. When the baby is stable you will be encouraged to change diapers, give baths, dress your baby and eventually learn all the care needed for your baby to prepare for discharge. Babies love to be read to, so please bring books from home if you have them, or ask your nurse for information about books for babies.
It depends on your baby, but a baby born with CDH typically spends two to three months in the hospital. Babies who need ECMO or have persistent pulmonary hypertension may require longer hospital stays than babies who do not require this level of support.
The strength of a CDH program comes from the depth and breadth of its team. Our team provides care from diagnosis through delivery, to the NICU and through childhood. Our interdisciplinary team is committed to working together for your baby and family. Your child’s care team is comprised of pediatric surgeons, neonatologists, advanced practice nurses, specialized surgical registered nurses, respiratory therapists, and nutritionists. Families are encouraged to be part of daily bedside rounds and to advocate for their baby every step of the way.
You will meet with a social worker after your initial evaluation to discuss how we can support you and your family during this time. Our team also has a psychologist and child life therapists, music therapists, chaplains and social workers who are available to you and your family — they can help any other children cope with the hospitalization of their new sibling. There are multiple unit-based support groups for you during and after your pregnancy.
Growth and feeding are the main concerns with babies with CDH. Some babies might require medication to help with reflux. Babies with CDH may need to go home on medications for pulmonary hypertension. We track development closely to provide any needed support to meet growth and developmental milestones.
CHOP’s Pulmonary Hypoplasia Program (PHP Program) is dedicated to the follow up care of babies born with CDH. Through this program, your child will be seen by an interdisciplinary team of specialists, including a pediatric surgeon, pediatric surgery nurse practitioner, pediatrician, pulmonologist, cardiologist, neonatologist, nutritionist, and physical, occupational and speech therapists. Social workers and a psychologist are also available to support your family. The clinic is arranged so that your child can see multiple specialists all in one day, at specific intervals based on their age and development.
A consistent team follows your baby into childhood. Any needs your baby has will be closely followed and treated in partnership with your family. Together, we celebrate the victories and find solutions to the problems.
CHOP’s CDH treatment team was recently recognized as a CHOP Frontier Program, a designation that supports our ongoing research efforts. We are focused on optimizing all phases of CDH care clinically from diagnosis through long-term follow up. Through our PHP Program, we follow more than 600 patients with CDH, and the knowledge gained from their outcomes informs ongoing innovations in care.
For more than 25 years, we have had an active translational research laboratory focused on lung development, gene editing, modes of ECMO and the use of alternative ventilator interfaces, and we are continuing our work to push the boundaries of clinical interventions for our patients.
In 2021, results published from the Tracheal Occlusion to Accelerate Lung Growth (TOTAL) Trial established that tracheal occlusion offers benefits in severe cases of prenatally diagnosed CDH.
Watch this video to learn about advances in CDH care pioneered by CHOP since 1995 and how we continue to push treatment to new frontiers and improve the life course for children.