Katie is a happy 2-year-old who loves listening to music, playing a toy drum, looking at flashcards, reading stories with her parents, and holding her 10-month-old brother.
Like every child, Katie has made amazing progress in the first years of life. And as a child with trisomy 21 (Down syndrome), she faces additional challenges.
After she was officially diagnosed with trisomy 21 when she was 3 weeks old, Katie became a patient of The Children's Hospital of Philadelphia's Trisomy 21 Program. This team of doctors, nurses and other experts offers specialized care to maximize the physical health and cognitive development of children with Down syndrome, whose unique needs include increased risk of heart defects.
Referral to CHOP's Cardiac Center for a heart murmur
 When Katie was 3 months old, her primary care pediatrician heard a heart murmur during a checkup. The pediatrician recommended the Cardiac Center at The Children's Hospital of Philadelphia, and Katie's parents, Colleen and Jay, felt confident returning to CHOP.
When Katie was 3 months old, her primary care pediatrician heard a heart murmur during a checkup. The pediatrician recommended the Cardiac Center at The Children's Hospital of Philadelphia, and Katie's parents, Colleen and Jay, felt confident returning to CHOP.
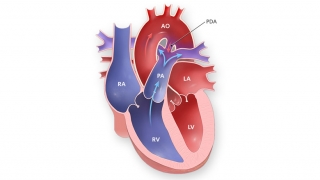
The family met with pediatric cardiologist Marie M. Gleason, MD. Based on the sound of the murmur and other factors, Dr. Gleason diagnosed Katie with patent ductus arteriosus (PDA), which occurs when a blood vessel in the fetal heart that is supposed to close after the baby is born remains open.
More About PDA
If the PDA isn't compromising the child's health, doctors wait to see if it will close on its own. In children with trisomy 21, though, PDAs are less likely to close. However, because Katie was not experiencing symptoms such as shortness of breath, Dr. Gleason assured her parents that the best approach was to monitor, rather than immediately treat, the abnormality.
"This whole process has been made easier because she is so good, and so forthcoming with information," Katie's mom says of Dr. Gleason.
Follow-up care
Katie visited Dr. Gleason every three months in Philadelphia or at the CHOP's Specialty Care Center in Exton, PA, for exams, echocardiograms and electrocardiograms.
"We were all hopeful the PDA would go away, but it did not," Colleen recalls. "When she was about 12 months old, Dr. Gleason said it was time to start thinking about fixing it."
Cardiac catheterization as a treatment
In most cases, small PDAs don't require surgery. Instead, they're treated with an interventional cardiac catheterization. Catheterization is often thought of as a diagnostic tool, but it is increasingly used as a less invasive form of treatment than heart surgery.
During catheterization, patients are under general anesthesia while the doctor threads a thin tube into the heart through a vein in the patient's groin area. Then, the doctor uses small coils or other devices, delivered by special catheters, to treat the defect.
On Oct. 28, 2008, at 6 a.m., Colleen and Jay brought Katie to the Hospital for the catheterization.
"We were just scared and very nervous," Colleen recalls. "We didn't know what to expect. Anytime you have to put your 18-month-old under anesthesia, that's stressful. But knowing the long-term benefits, we knew it was the right thing to do."
With Katie's parents by her bedside, three nurses in the Cardiac Preparation and Recovery Unit placed an IV line and helped get Katie ready. Colleen and Jay walked beside Katie's bed as the team wheeled her to the catheterization lab down the hall. After Matthew Gillespie, MD, who would perform the procedure, introduced himself, Katie's parents said goodbye.
Dramatic change after catheterization
A little more than an hour later, the catheterization was complete. Dr. Gillespie came to the waiting room and explained the procedure.
"What was amazing to us were the 'before and after' pictures he showed us on a computer," Katie's mom says. "You could see the blood flowing out of her heart where it should not have been. And he showed us the next picture, after he placed the [device], and the blood was no longer flowing out."
After Katie woke up, Cardiac Center nurse Lauren Clark, RN, carefully monitored her for six hours before the family could go home.
"Our nurse was phenomenal," Colleen says. "Really, really diligent and very, very caring. To work at CHOP, it takes a special person, and she was just very good."
Follow-up care
Six months after the procedure, Katie's health is excellent. She has had two follow-up appointments with Dr. Gleason, and will have another in two years.
In addition to the care Katie and her family will continue to receive from the Cardiac Center, they visit Tahira G. Adeleken, MD, a developmental pediatrician in the Trisomy 21 Program, at least once a year. And Katie and her mom come to CHOP once a week for aquatic therapy with an occupational therapist.
"We have had a wonderful experience with everyone at CHOP," Colleen says. "Because of what they've been able to do for Katie, I always trust them and I know she's in good hands. I never felt like anyone was glossing over the diagnoses."
“They understand how difficult this is for parents. The empathy and the understanding are always there.”
Originally posted: June 2009