Natasha will never forget looking at the ultrasound at her obstetrician’s office when she was five months pregnant with her first child.
She had been working for the Cardiac Center at Children’s Hospital of Philadelphia for three years, as a respiratory therapist, and she knew immediately: her baby had a severe congenital heart defect.
“They had her heart up on a screen and I could tell she was a hypoplast,” she remembers. “I was petrified.”
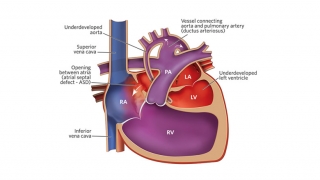
 “Hypoplast” is a term for a patient with hypoplastic left heart syndrome (HLHS), in which the left side of the heart is underdeveloped. After the ultrasound, Natasha called to tell her friends and colleagues the news.
“Hypoplast” is a term for a patient with hypoplastic left heart syndrome (HLHS), in which the left side of the heart is underdeveloped. After the ultrasound, Natasha called to tell her friends and colleagues the news.
For the next four months, as she continued working in the Cardiac Center, Natasha was also a patient.
She visited the Fetal Heart Program staff every two weeks at first, and then every week. The Fetal Heart Program at CHOP specializes in the detection, evaluation and management of fetal heart defects prior to a baby's birth.
The team made a plan for delivery, and educated Natasha about what to expect with Caila’s HLHS: a series of three open heart surgeries, known as staged reconstruction. “They gave us the rundown without having it be too overwhelming,” Natasha says.
Delivery day
Caila was born full-term on Nov. 16, 2000, weighing 7 pounds and 10 ounces. Delivered at the Hospital of the University of Pennsylvania at 7:01 p.m., she was immediately taken next door to Children’s Hospital, where a team was waiting.
More About HLHS
If Caila were born today, she may have been delivered in Children’s Hospital’s Garbose Family Special Delivery Unit (SDU), a state-of-the-art labor and delivery unit for mothers carrying babies with known birth defects. The unit is on the same floor as the cardiac units, so parents and baby stay close.
“It’s hard to have a baby and not be able to hold her,” Natasha recalls. “That’s what’s great about the SDU. They’re right here.”
Caila’s father, George, visited her that night and Natasha was able to see her the next morning.
“They had put a little bow in her hair,” she recalls. “They doted on her. It was like they were taking care of one of their own.”
That was a Friday. Caila's first open heart surgery would be Monday.
“We had her baptized and my parents came down,” Natasha recalls. “We got to hold her. Monday was the hardest day of my life by far.”
HLHS repair
When Caila was only 3 days old, she had the stage I operation needed for hypoplastic left heart syndrome, known as the Norwood procedure. During the four-hour procedure, Thomas Spray, MD, created a Blalock-Taussig shunt, connecting another artery to the pulmonary artery to allow extra blood flow to the lungs. He also enlarged Caila’s aorta, which was abnormally small.
Caila spent 12 days in the Hospital. After she came home, she had difficulty eating at first, but gradually began to gain weight.
When Caila was 3 months old, Natasha returned to work full-time. She educated the daycare staff about Caila’s HLHS and verified that they were CPR-certified.
Caila had her second HLHS surgery, the stage II operation known as the bidirectional Glenn, at 5 months. She then had the stage III operation, known as the Fontan procedure, at 18 months.
Her circulatory system was reconfigured so that deoxygenated blood that has circulated through her body flows directly to her lungs. Normally, this blood would flow into the right side of the heart and be pumped to the lungs. In patients with HLHS, after the series of surgeries, the right side of the heart does what is normally the job of the left side — pumping oxygenated blood to the body — because the left side is too underdeveloped to function.
Caila today
Nearly 15 years have passed since Caila’s last surgery and today she’s thriving. "She's reaching milestones we were never sure would happen," says her mom. Caila is a sophomore in high school, and that means she’s celebrating her Sweet Sixteen, ordering her class ring, and learning to drive.
“It’s all these things that she doesn’t even realize are a big deal, but to me, it’s amazing to see her growing up..”
Caila is very active. She dances at ballet class and participates in gym class. She sings with her school choir. And she loves taking trips to New York City to see Broadway shows.
As she gets older, Caila is learning to manage her own healthcare needs. She now visits CHOP just every six months, but her medical team is there for her when she experiences the occasional setback, like feeling fatigued or short of breath.
Hope for the future
Thirty years ago, children born with HLHS couldn’t survive. Hypoplastic left heart syndrome survival rate is much higher in children today due to great strides in research and care at pediatric institutions such as The Children’s Hospital of Philadelphia.
“To see the patients go home and thrive, that’s a huge change,” Natasha says. “My experience has made me appreciate where I work even more."
Originally posted: November 2009
Updated: November 2016