When Spinal Surgery Can Improve Mobility for Children with Spastic Diplegic Cerebral Palsy
Published on
Children's DoctorPublished on
Children's DoctorNivedita Thakur, MD, Joseph Vithayathil, MD, PhD, Benjamin Kennedy, MD, and Andrea O’Brien, MSN, CRNP
Case: A 3-year-old female with a history of 31-week prematurity, grade III intraventricular hemorrhage, congenital hypothyroidism, subglottic stenosis, cleft palate, and retrognathia presented to Neurology for evaluation of gross motor delays. She was referred to Neurology because her Orthopedic surgeons had concern for cerebral palsy due to her abnormal lower extremity tone and range of motion deficits that limited her ability to walk.
Functionally, she was independent with floor mobility, primarily relying on tall knee walking and crawling through the home. She used a posterior rolling walker for long distances and to navigate her preschool setting. Her fine motor and speech skills were assessed as developmentally appropriate. Based on her neurology exam, she was found to have bilateral heel cord tightness and toe walking. She had spasticity of her lower extremities and normal tone of her upper extremities. She was given a diagnosis of spastic diplegic cerebral palsy and referred to rehabilitation for further evaluation of her muscle tone.
Her rehabilitation evaluation demonstrated spasticity of adductors, hamstrings, and heel cords. Rehabilitation recommended Botox® injections and serial casting with physical therapy. She underwent multiple rounds with improvement in range of motion and function. However, due to underlying spasticity, these results were difficult to maintain.
At age 5, she was independent with a walker and used crawling or cruising to navigate tight spaces at home. Due to her spasticity and contractures in her lower legs, she was unable to achieve appropriate foot contact for balance and her gross motor function was consistent with Gross Motor Function Classification System (GMFCS) level II (see Table 1). She was evaluated by the team at Advanced Tone Management (ATM) Multidisciplinary Clinic at Children’s Hospital of Philadelphia for a selective dorsal rhizotomy (SDR), a surgical procedure that selectively thins the nerves running from the spinal cord to the legs.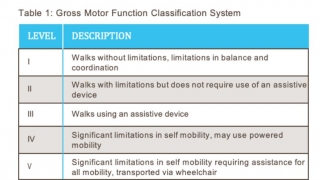
As part of the work up, we reviewed her brain MRI to confirm the findings (see Figure 1) referred to as periventricular leukomalacia (PVL). PVL is seen as a sequelae of hypoxic/ischemic injury or intraventricular hemorrhage that can occur in premature babies. She was found to be a good candidate due to diplegic tone, age, and cognitive ability to follow directions and participate in therapies, which is required for a good post-op outcome.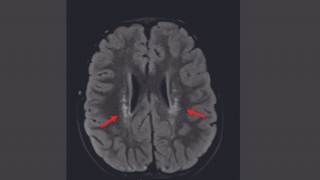 Figure 1: FLAIR MRI of the brain demonstrating T2 hyperintensities (arrows) consistent with the periventricular leukomalacia commonly found in cerebral palsy that led to spastic diplegia in this patient.
Figure 1: FLAIR MRI of the brain demonstrating T2 hyperintensities (arrows) consistent with the periventricular leukomalacia commonly found in cerebral palsy that led to spastic diplegia in this patient.
She underwent SDR at age 5 and spent 5 weeks in inpatient rehab for intensive physical and occupational therapy. Her tone significantly improved immediately after surgery. She continued outpatient physical therapy 2 to 3 times weekly, and school-based physical therapy 1 to 2 times weekly for 1 year. At her 1-year evaluation, she was walking with a more normalized gait pattern and taking up to 20 steps without any assistive device.
Discussion: SDR is a surgical procedure performed on the lower spine (1-level laminectomy) to reduce spasticity in the legs of children who have a spastic form of cerebral palsy. SDR corrects muscle spasticity by cutting some of the sensory nerve rootlets in the spinal cord that are sending abnormal signals to the muscles. See Figure 2. Reducing the spasticity allows for improved motor control of the legs, and ultimately an improvement in how a child stands and walks.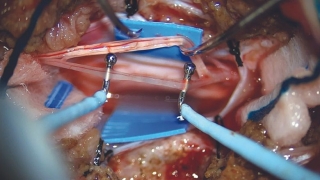 Figure 2: Microscopic view through a narrow 1-level L1 laminectomy. Each root is dissected into several fascicles to determine which ones are responsible for the most spasticity.
Figure 2: Microscopic view through a narrow 1-level L1 laminectomy. Each root is dissected into several fascicles to determine which ones are responsible for the most spasticity.
The best candidates for SDR surgery typically have cerebral palsy that affects the legs more than the arms and are walking in some capacity, with or without an assistive device. It is important to screen to make sure their tone is primarily related to spasticity and not dystonia. Dystonia refers to fluctuating tone in which patients’ muscle may be relaxed and at other times appear very tight and have muscle posturing. Patients who have mainly dystonia would not benefit from this procedure. Children ages 4 to 10 years old are typically ideal candidates, but older children may benefit, and each will be evaluated on an individual basis. Children must be cognitively able to participate in therapy and follow directions because SDR requires extensive rehabilitation to ensure a good outcome.
Children with severe spasticity in their arms and legs may also be candidates. For these children, the goal of SDR is for ease of care by caregivers, and to reduce the patient’s pain and increase independence, enabling them to sit for longer periods, or to control movement in a wheelchair.
Each potential candidate will undergo an evaluation by our ATM Clinic team, which includes members from rehabilitation medicine, neurology, neurosurgery, physical therapy, occupational therapy, nursing, and social work—all with expertise in pediatric patients with increased tone.